背景
对于低度侵犯的早期肾细胞肾癌(RCC)来说,经皮穿刺微波消融术(MWA)和经腹腔镜部分切除术(LPN)是两种符合适应症的治疗手段。
目的
比较经皮穿刺MWA与LPN在治疗cT1a RCC的远期结果。
材料与方法
本研究回归性分析了1955例cT1a RCC且经经皮穿刺MWA或LPN治疗的患者。利用倾向匹配方法进行比较。利用Fine-and-Gray竞争风险模型分析肿瘤预后结果。
结果
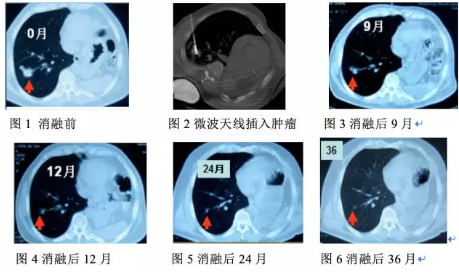
共有185例患者行经皮穿刺MWA,共有1770例患者行LPN。在随访过程中(中位数为40.6个月),经过倾向评分匹配,在两组间局部肿瘤进展(3.2% vs 0.5%, P = .10),、肿瘤特异性生存期(2.2% vs 3.8%, P = .24)和远期转移(4.3% vs 4.3%, P = .76)间并无显著差异性。行经皮穿刺MWA的患者的整体生存期(hazard ratio, 2.4; 95% confidence interval: 1.0, 5.7; P = .049 vs LPN)和无肿瘤生存期(82.9% vs 91.4%, P = .003)要比LPN组差。与LNP组相比,经皮穿刺MWA患者在出院时估算肾小球滤过率下降较小(6.2% vs 16.4%, P < .001)、出血量较小(4.5 mL ± 1.3 vs 54.2 mL ± 69.2)、治疗费用较低($3150 ± 2970 vs $6045 ± 1860 U.S. dollars)、手术时间短(0.5 minute ± 0.1 vs 1.8 minutes ± 0.6)、术后住院时间短(5.1 days ± 2.6 vs 6.9 days ± 2.8) (all P < .001 vs LPN)。经皮穿刺MWA组术后发热率较小。
结论
关于预后和并发症,经皮穿刺微波消融术和经腹腔镜部分切除术在治疗cT1a RCC患者间并无显著性差异。经皮穿刺微波消融术具有对肾功能损伤小、失血量少的独特的。对于不能接受侵入性更大的腹腔镜部分切除术的患者来说,经皮穿刺微波消融术是一个不错的选择。
原始出处:
Yu J, Zhang X, Liu H. et al. Percutaneous Microwave Ablation versus Laparoscopic Partial Nephrectomy for cT1a Renal Cell Carcinoma: A Propensity-matched Cohort Study of 1955 Patients.
DOI: 10.1148/radiol.2020190919
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








学习
65
#肾细胞肾癌#
40
#切除术#
30
#腹腔镜#
41
#消融#
26
#消融术#
34
#消融术#
41