N Engl J Med:多学科讨论:贝伐珠单抗为洛莫司汀治疗胶质母细胞瘤锦上添花?
2017-12-26 应颖秋 环球医学
尚未确立进行性胶质母细胞瘤患者的治疗标准。2017年发表在《N Engl J Med》的一项研究考察了洛莫司汀+贝伐珠单抗治疗进行性胶质母细胞瘤的效果。请看本期多学科讨论组临床药师各抒己见为您梳理本文看点——
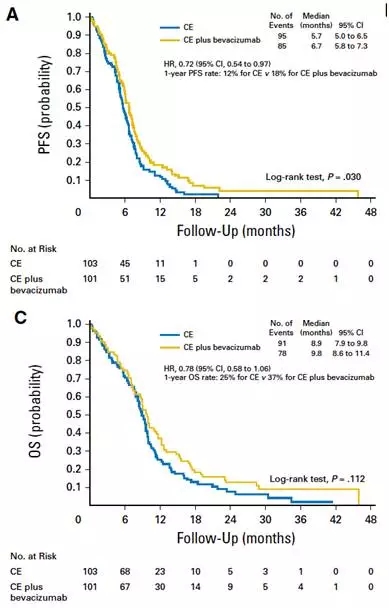
背景:基于非对照数据,贝伐珠单抗获准用于进行性胶质母细胞瘤患者的治疗。2期试验数据表明,与洛莫司汀单一治疗相比,将贝伐珠单抗添加到洛莫司汀中,可改善总生存期。研究者旨在确定,首次胶质母细胞瘤进展的患者中,联合治疗是否比洛莫司汀单一治疗具有更长的总生存期。
方法:研究者将放化疗后进展的患者按照2:1的比例随机分配到洛莫司汀+贝伐珠单抗组(联合治疗组,288人)或洛莫司汀单一治疗组(单一治疗组,149人)中。研究者评估了O6-甲基鸟嘌呤DNA甲基转移酶(MGMT)启动子的甲基化状态。于基线和每12周评估了健康相关生活质量和神经认知功能。首要终点为总生存期。
结果:总共随机分组了437例患者。联合治疗组和单一治疗组的患者分别接受了3个和1个为期6周的治疗周期。在329例总生存事件(75.3%)中,联合治疗组未显示出生存期优势:联合治疗组和单一治疗组的中位总生存期分别为9.1个月(95% 置信区间[CI],8.1~10.1)和8.6个月(95% CI,7.6~10.4)(死亡的风险比,0.95;95% CI,0.74~1.21;P=0.65)。联合治疗组比单一治疗组局部评估的无进展生存期长2.7个月:4.2 vs 1.5个月(疾病进展或死亡的风险比,0.49;95% CI,0.39~0.61;P<0.001)。联合治疗组和单一治疗组分别有63.6%和38.1%的患者发生3~5级不良事件。将贝伐珠单抗添加到洛莫司汀中既不影响健康相关生活质量,也不影响神经认知功能。MGMT状态可预测预后。
结论:尽管一定程度上会延长进行性胶质母细胞瘤患者无进展生存期,但是洛莫司汀+贝伐珠单抗并没有比洛莫司汀单一治疗显示出更好的生存优势。
多学科讨论记实:
EORTC 26101提供了贝伐珠单抗在进行性胶质母细胞瘤患者中的疗效的3期数据。贝伐珠单抗+洛莫司汀并不产生优于洛莫司汀单药的生存优势,但微微延长无进展生存期。此获益在试验的评估中一致,尽管有一些地区和中心差异,EORTC 26101显示出在一项国际神经肿瘤学试验中应用统一MRI方案的可行性。
尽管BRAIN试验(关于复发性胶质母细胞瘤患者)和Avastin in Glioblastoma试验(关于新确诊胶质母细胞瘤患者)的早期报告显示,贝伐珠单抗有减少糖皮质激素的效果,在当前试验中添加贝伐珠单抗并不使糖皮质激素使用减少。MGMT状态不预测联合治疗的获益。既往数据显示,洛莫司汀对MGMT未甲基化的胶质母细胞瘤作用很小,添加贝伐珠单抗不改变这一结论。
EORTC不能证实2期试验的就结论——贝伐珠单抗添加到洛莫司汀可改善进行性胶质母细胞瘤患者的生存。对无进展生存期的影响与总生存率增加无关,联合治疗与毒性增加相关。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#胶质母细胞#
31
#Eng#
28
#Engl#
37
#母细胞瘤#
35
#贝伐珠#
28
#多学科#
33
#细胞瘤#
29
#贝伐#
36
#Med#
33