JAMA Oncol:阿帕替尼 vs安慰剂治疗局部晚期或转移性、放射性碘难治分化型甲状腺癌患者的疗效: 随机临床研究REALITY
2021-12-22 yd2015 MedSci原创
REALITY研究表明,阿帕替尼较安慰剂明显改善放射性碘难治性分化型甲状腺癌的PFS和OS。
放射性碘难治分化型甲状腺癌患者的预后较差,而且可选择的治疗方式比较局限。因此,来自北京协和医院和南京中医药大学的团队开展了一项III期随机临床研究REALITY (NCT03048877), 评估阿帕替尼对比安慰剂治疗局部晚期或转移性、放射性碘难治分化型甲状腺癌患者的疗效和安全性。相关结果发表在JAMA Oncology杂志上。
REALITY研究是2017年2月17日至2020年3月2日期间在中国的21个中心进行的一项随机、双盲、安慰剂对照的III期临床研究。患者1:1随机分配至接受阿帕替尼(500mg/日)和安慰剂治疗。主要研究终点为PFS,次要研究终点为OS,ORR,DCR,DOR和安全性。
研究纳入的92例患者中,56例为女性(60.9%);基线时的平均(SD)年龄为55.7(10.6)岁。患者被随机分为阿帕替尼组(n = 46)和安慰剂组(n = 46)。中位随访时间为18.1个月(IQR,12.7-22.2)。阿帕替尼的中位PFS为22.2个月(95%CI,10.91-未达到),安慰剂组为4.5个月(95%CI,1.94-9.17)(HR=0.26;95%CI,0.14-0.47;P<0.001)。阿帕替尼组12个月和24个月PFS率分别为60.3% (95% CI, 40.8%-75.2%)和37.2% (95% CI, 15.1%-59.7%),安慰剂组分别为12.4% (95% CI, 3.4%-27.4%)和4.1% (95% CI, 0.3%-17.2%)。
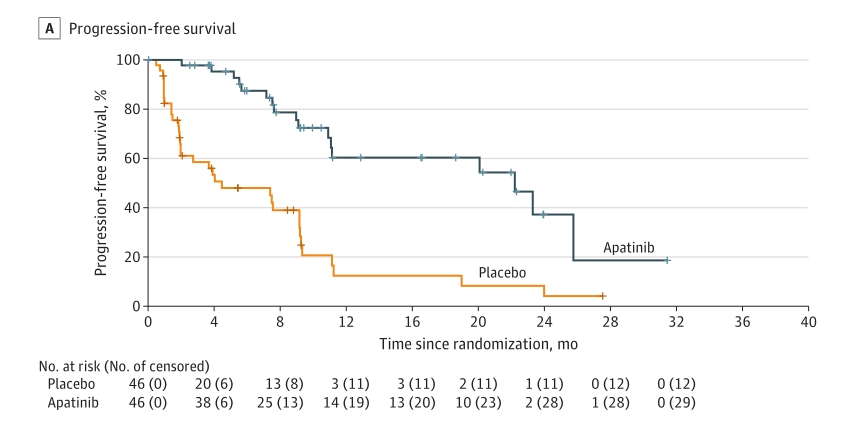
PFS
阿帕替尼组的ORR为54.3%(95%CI,39.0% -69.1%)和DCR为95.7%(95%CI,85.2% -99.5%);而安慰剂组的ORR为2.2%(95%CI,0.1% -11.5%)和DCR为58.7%(95%CI,43.2% -73.0%)。此外,阿帕替尼组25例确认有应答的患者中位到达出现客观应答的时间为1.9个月(IQR, 1.2-3.7), DOR为22.4个月(95% CI, 17.7-27.1)。
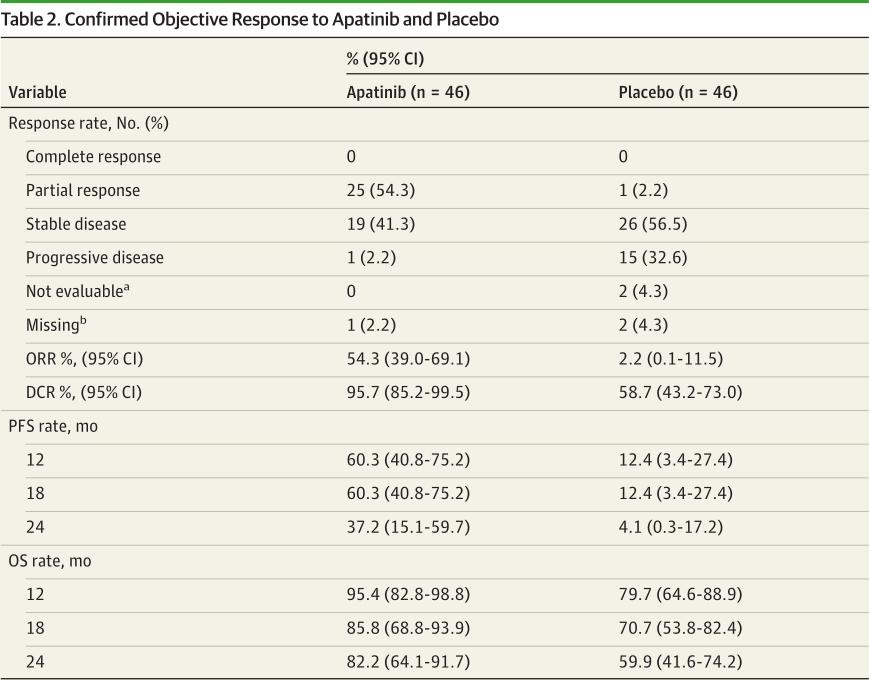
疗效评估
阿帕替尼的中位OS尚未达到(95%CI,26.25-未达到),安慰剂组的中位OS为29.9个月(95%CI,18.96-未达到)(HR=0.42;95%CI,0.18-0.97;P =0.04)。
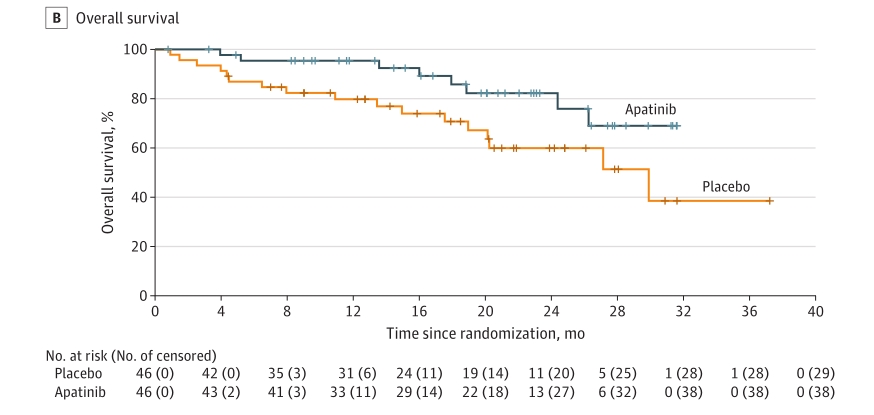
OS
阿帕替尼组最常见的3级或更高级别的治疗相关不良事件是高血压(16[34.8%])、手足综合征(8[17.4%])、蛋白尿(7[15.2%])和腹泻(7[15.2%]),而安慰剂组中没有发生这些不良事件。
综上,REALITY研究表明,阿帕替尼较安慰剂明显改善放射性碘难治性分化型甲状腺癌的PFS和OS。
原始出处:
YansongLin, ShukuiQin, ZhiyongLi, et al. Apatinib vs Placebo in Patients With Locally Advanced or Metastatic, Radioactive Iodine–Refractory Differentiated Thyroid Cancer: The REALITY Randomized Clinical Trial. JAMA Oncol.doi:10.1001/jamaoncol.2021.6268. Published online December 16,2021.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#局部晚期#
51
#Oncol#
34
#安慰剂#
57
#分化型甲状腺癌#
45
#转移性#
31
#放射性碘#
59
#局部#
35