Cancers:真实世界研究表明在阿法替尼基础上加用贝伐珠单抗并不能显著改善EGFR敏感突变NSCLC患者的预后
2022-01-10 yd2015 MedSci原创
真实世界数据表明,在阿法替尼基础上加用贝伐珠单抗并不能显著改善EGFR敏感突变NSCLC患者的预后。
阿法替尼单药或联合贝伐单抗治疗表皮生长因子受体(EGFR)突变的非小细胞肺癌(NSCLC)患者的疗效尚不明确。因此,来自我国台湾的学者开展了真实世界研究,评估阿法替尼单药或联合贝伐单抗治疗EGFR突变的NSCLC患者的疗效。相关结果发表在Cancers杂志上。
共有405名EGFR敏感突变的晚期NSCLC患者接受一线阿法替尼单药或联合贝伐单抗治疗,并进行了分组和倾向评分匹配。分析无进展生存期(PFS)、总生存期(OS)和继发性T790M突变。
纳入405例患者中,其中367例(90.6%)患者接受阿法替尼单药治疗,38例(9.4%)患者接受阿法替尼联合贝伐单抗治疗。经过PSM匹配后,包括152例患者,其中单药组34例,联合组有118例患者。
阿法替尼联合贝伐单抗和阿法替尼单药组的中位随访时间分别为23.5个月和37.8个月。联合组的颅内反应率和颅内疾病控制率分别为38.5%和100.0%,单药阿法替尼组的颅内反应率和颅内疾病控制率分别为60.6%和93.9%。

疗效评估
中位无进展生存期(16.1 vs. 15.0个月;log-rank检验p = 0.500),疾病进展风险降低(HR 0.85 [95% CI, 0.52-1.40];p = 0.528))和24个月无进展生存率(40.9% [95% CI, 25.6%-65.3%]vs. 32.2% [95% CI, 24.6%-42.3%])在联合治疗组和单药治疗组之间相似。中位OS (32.1 vs. 42.0个月;log-rank检验p = 0.700),死亡风险降低(HR 0.85 [95% CI, 0.42 -1.74];p = 0.660))和24个月OS率(73.7% [95% CI, 57.3%-94.7%]vs 67.2% [95% CI, 59.1%-76.5%])在两组之间也类似。
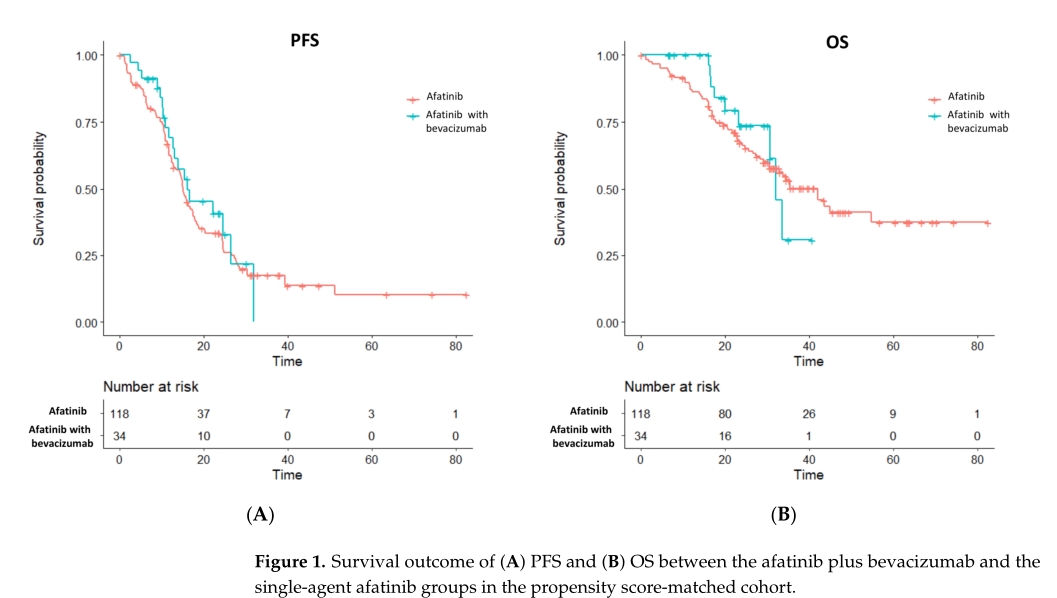
PFS和OS
男性患者(HR 0.56 [95% CI, 0.23-1.35];p = 0.198),≥65岁患者(HR 0.51 [95% CI, 0.17-1.51];p = 0.222),以及有肝转移的患者(HR 0.57 [95% CI, 0.19-1.72];p = 0.318)加用上贝伐珠单抗并不能改善PFS。

PFS亚组分析
男性患者(HR 0.58 [95% CI, 0.13 2.63];p = 0.486), EGFR L858R突变患者(HR 0.65 [95% CI, 0.19 2.17];p = 0.485),以及没有出现脑转移的患者(HR 0.53 [95% CI, 0.16 1.75];p = 0.296)中加上贝伐珠单抗并不能改善患者OS。
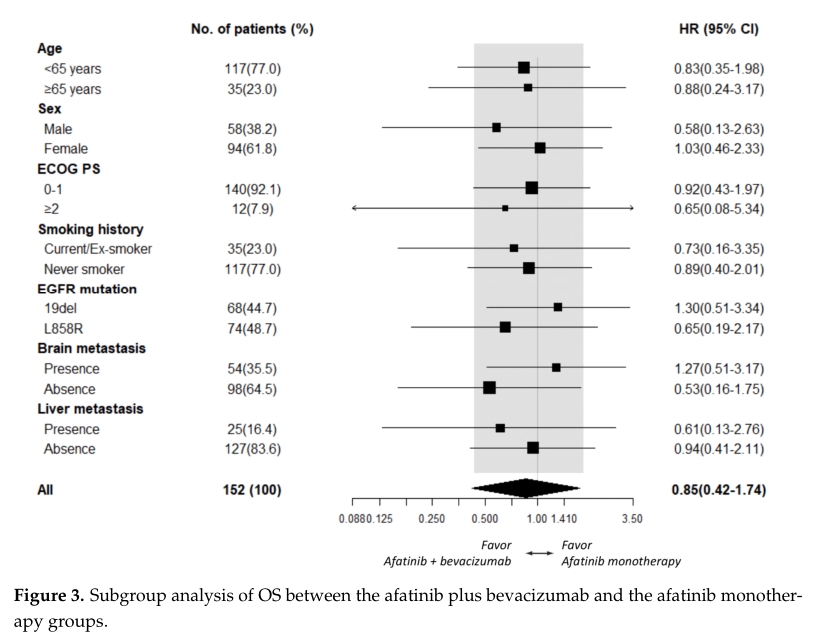
OS亚组分析
在405例患者中,数据分析时279例(68.9%)患者出现疾病进展。共有170例(42.0%)患者接受组织或液体活检,其中85例(50.0%)患者诊断为T790M突变阳性。T790M阳性率在阿法替尼加贝伐单抗组和阿法替尼单抗组之间相似(56.3% vs 49.4%,p = 0.794)。单因素分析显示男性(OR 0.61 [95% CI, 0.33 1.13];p = 0.122), EGFR L858R突变(OR 0.62 [95% CI, 0.33 1.16];p = 0.137), EGFR罕见突变(OR 0.21 [95% CI, 0.03 0.94];p = 0.063)与T790M-阳性率较低相关,而PFS长于12个月(OR 2.40 [95% CI, 1.27 4.60];p = 0.008)与T790M阳性较高相关。在多因素分析中,EGFR L858R突变(OR 0.51 [95% CI, 0.26 0.97];p = 0.044), EGFR罕见突变(OR 0.14 [95% CI, 0.02 0.64];p= 0.021),且PFS长于12个月(OR 2.71 [95% CI, 1.39 5.41];p = 0.004)仍然是T790M阳性的独立预测因子。
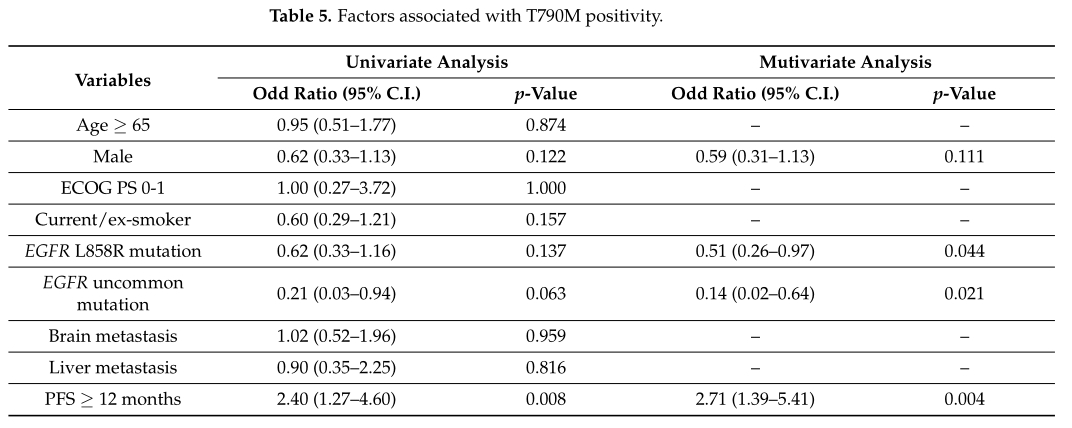
T790M突变阳性相关因素
综上,真实世界数据表明,在阿法替尼基础上加用贝伐珠单抗并不能显著改善EGFR敏感突变NSCLC患者的预后。
原始出处:
Kuo, C.-H.S.; Chiu, T.-H.;Tung, P.-H.; Huang, C.-H.; Ju, J.-S.;Huang, A.C.-C.; Wang, C.-C.;Ko, H.-W.; Hsu, P.-C.; Fang, Y.-F.; et al.Afatinib Treatment Alone or with Bevacizumab in a Real-World Cohort of Non-Small Cell Lung Cancer Patients with Epidermal Growth Factor Receptor Mutation. Cancers.2022, 14, 316. https://doi.org/10.3390/cancers14020316
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#EGFR敏感突变#
38
#ERS#
36
#EGFR敏感#
49
#贝伐珠#
36
#SCLC患者#
51
#真实世界#
24
#NSCLC患者#
33
#贝伐#
25
#GFR#
31
学习了,谢谢分享
42