Dig Dis Sci:新诊断为炎症性肠病的年轻患者的骨密度明显偏低
2021-02-09 MedSci原创 MedSci原创
以溃疡性结肠炎(UC)和克罗恩病(CD)为主的炎症性肠病(IBD)被认为是胃肠道的慢性非特异性炎症。这种情况可能导致营养物质吸收不良,并引起并发症。
以溃疡性结肠炎(UC)和克罗恩病(CD)为主的炎症性肠病(IBD)被认为是胃肠道的慢性非特异性炎症。这种情况可能导致营养物质吸收不良,并引起并发症,例如骨质减少和骨质疏松。许多报告表明,与普通人群相比,IBD患者的骨质疏松症和骨质疏松症患病率较高,双能X射线骨密度仪(DXA)可以估算骨密度(BMD),而骨矿物质密度在确定骨强度中起着不可或缺的作用。许多研究人员认为,低BMD的临床危险因素是小肠切除术史,低体重指数(BMI),使用皮质类固醇激素,营养不良(包括钙和维生素D缺乏),IBD的病程以及吸烟等等。IBD患者低BMD的发病机制是多因素的,尚未完全揭示。因此,本项研究旨在探究新诊断为IBD的韩国年轻患者中低BMD的患病率和危险因素。

研究人员在2014年11月至2017年4月之间从韩国6个三级转诊中心招募了132名年龄小于50岁且新诊断为IBD的患者。通过双能X射线吸收法测量BMD,然后确定Z评分。低BMD的定义为Z分数≤−1.0。然后对所有患者进行统计学分析。
在68例溃疡性结肠炎(UC)患者中,有22例(32.4%)处于BMD较低水平。另外,在64名克罗恩病(CD)患者中,有24名(37.5%)的BMD较低。多元回归分析的结果确定了UC患者低BMD的危险因素是碱性磷酸酶(ALP)水平较高(≥140 U / L)(P =0.010),以及体重过轻(体重指数≤18.5 kg/m2)。
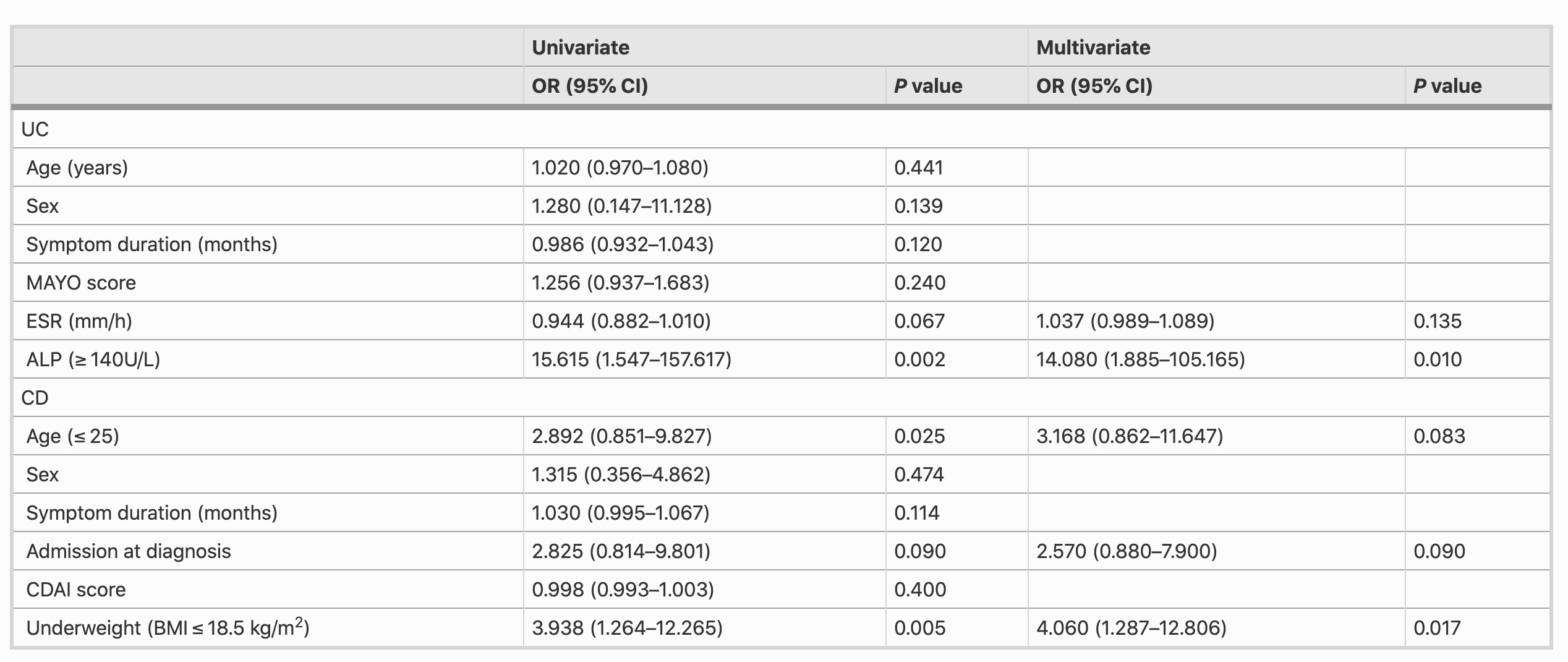
大约三分之一的新诊断为IBD的亚洲患者的BMD处于较低水平。与低BMD相关的临床因素是UC患者的ALP水平高,而CD患者是体重过轻。因此,在诊断IBD时应考虑对年轻患者的BMD进行测量。
原始出处:
Joon Seop Lee. Et al. Low Bone Mineral Density in Young Patients Newly Diagnosed with Inflammatory Bowel Disease. Digestive Diseases and Sciences.2021.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#新诊断#
41
#Dis#
35
#年轻患者#
50
#炎症性#
32