J Immunother Cancer:Nivolumab 联合 ipilimumab治疗晚期罕见妇科肿瘤的疗效和安全性:来自CA209-538临床研究
2021-11-20 yd2015 MedSci原创
研究表明,Ipilimumab和nivolumab联合治疗在晚期罕见妇科恶性肿瘤中具有显著的临床活性和良好的安全性,值得进一步研究。
罕见癌症患者占所有妇科恶性肿瘤的55%,由于治疗选择有限,预后很差。Nivolumab联合ipilimumab免疫治疗已在一系列常见恶性肿瘤中显示出显著的临床疗效。CA209-538是一项多中心多队列II期临床研究,评估联合抗PD- 1抗体nivolumab和抗CTLA- 4抗体ipilimumab对罕见肿瘤患者的疗效。近期,Journal for ImmunoTherapy of Cancer杂志上发表了CA209-538中该联合免疫方案在罕见妇科肿瘤的疗效和安全性。
这项多中心II期研究纳入了43例晚期罕见妇科肿瘤患者。患者接受nivolumab和ipilimumab诱导治疗,剂量分别为3mg /kg和1mg /kg,每3周一次,共4周期。继续使用nivolumab单药治疗,每2周3mg / kg,直到疾病进展或最长2年。主要终点是第12周疾病控制率(根据实体瘤疗效评价标准V.1.1,完全缓解、部分缓解或疾病稳定(SD))。对肿瘤程序性死亡配体1 (PD- L1)表达和肿瘤突变负荷(TMB)相关的临床结果进行探索性评估。

临床特征
总体而言,在数据分析时(2020年11月),43例患者中有20例(47%)存活,中位随访时间为16.8个月。30例(70%)患者完成了4周期nivolumab和ipilimumab的诱导治疗,10例(23%)患者在诱导治疗期间出现临床进展,其中大多数患者仅分别接受1或2剂治疗。3例(7%)患者在诱导期因高级别免疫相关不良事件(irAEs)而停止治疗。其中一名患者随后改用单药nivolumab治疗,另外两名患者在第一次再复发时因疾病进展而退出研究。在完成诱导治疗的30例患者中,20例患者应用nivolumab维持治疗,10例患者在第12周第一次放射学评估时因疾病进展而退出研究。
影像学可评估人群的客观缓解率为36%(12/33),意向治疗人群的客观缓解率为28%(12/43)。疾病控制率则分别为58%和44%。
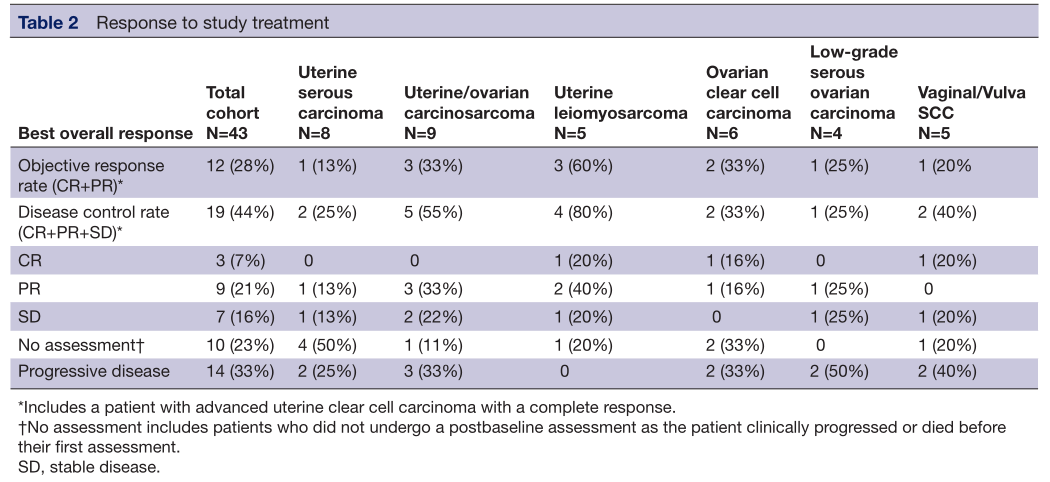
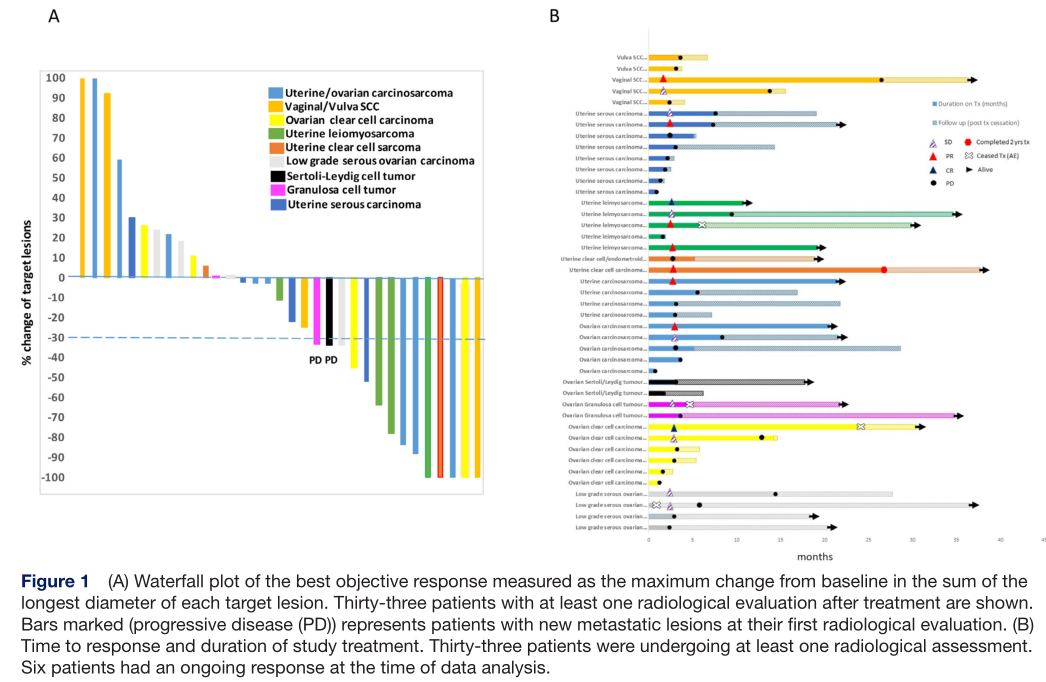
疗效评估
整个队列的中位无进展生存期(PFS)和总生存期(OS)分别为2.8个月(95% CI: 2.6 - 6.7)和15.8个月(95% CI: 5.8 - 19.1)。
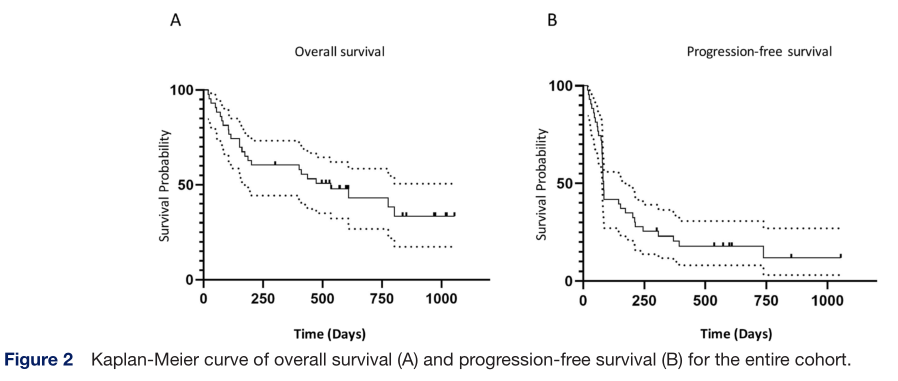
OS和PFS
总体而言,43例患者中有31例(72%)发生任何级别的免疫相关不良事件,7例(16%)患者发生3级或更高级别的免疫相关毒性。治疗相关的不良事件导致4例(9%)患者停止治疗。没有治疗相关的死亡病例。
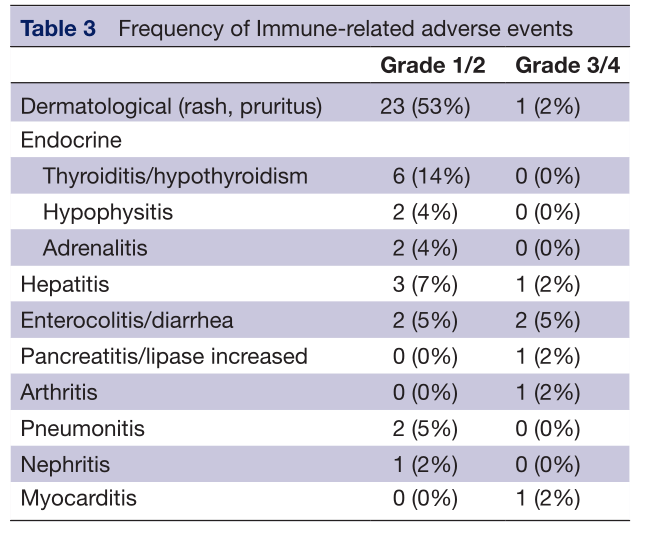
不良反应
24例(73%)患者的肿瘤细胞上至少有1%的PD- L1表达阳性,其中11例(46%)有客观反应。在9例PD- L1阴性肿瘤患者中,只有1例(11%)获得治疗反应。对所有33例患者的肿瘤进行肿瘤DNA测序以评估TMB。这些肿瘤中绝大多数的TMB小于10/ MB (MB),患者获得客观缓解与SD或疾病进展之间的中位TMB没有差异。
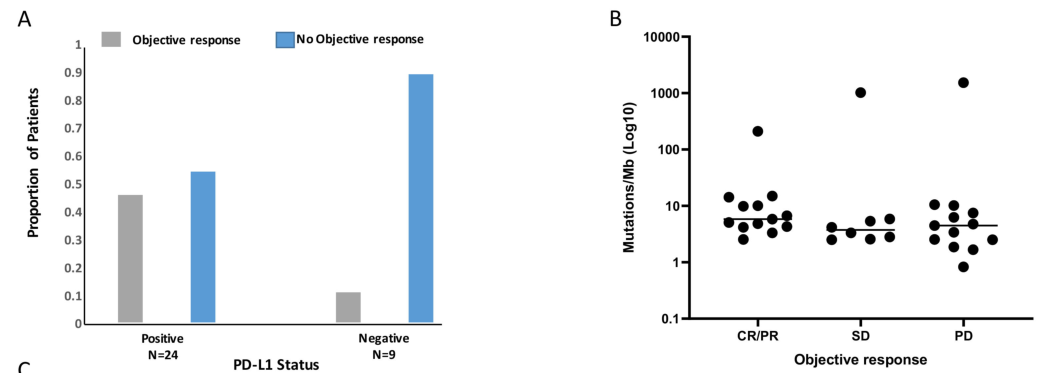
标志物探索
综上,研究表明,Ipilimumab和nivolumab联合治疗在晚期罕见妇科恶性肿瘤中具有显著的临床活性和良好的安全性,值得进一步研究。
原始出处:
Klein O, Kee D, Gao B, et al. Combination immunotherapy with nivolumab and ipilimumab in patients with rare gynecological malignancies: results of the CA209- 538 clinical trial. Journal for ImmunoTherapy of Cancer 2021;9:e003156. doi:10.1136/jitc-2021-003156
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#疗效和安全性#
41
#mAb#
32
#NIV#
29
#Ipilimumab#
36
#罕见#
34
#CA2#
36