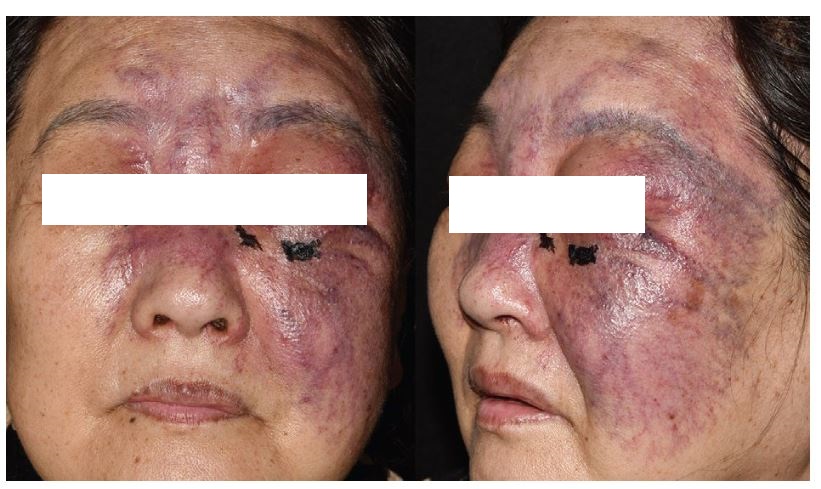
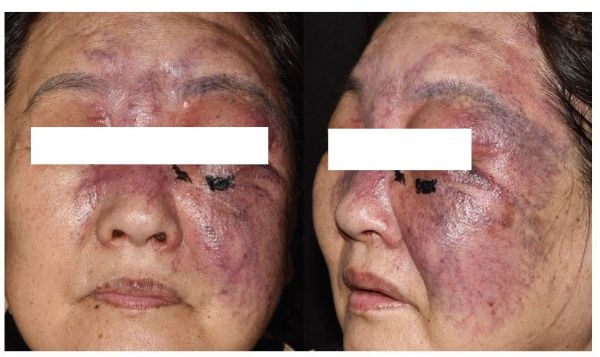
老年女性患者面部紫罗兰色肿胀伴毛细血管扩张和坏死1例
2019-04-27 王盼 皮肤周讯
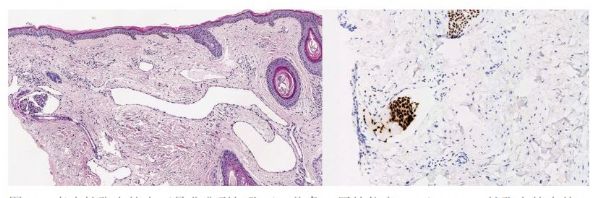
患者女性,60余岁,因面部3个月疼痛、肿胀和红斑就诊。11年前,患者被诊断为左乳腺癌,并接受了乳房切除术,随后进行了放疗和化疗。七年后,发现患者左锁骨处淋巴结转移,并进行了手术切除。在出现这些症状时,触诊发现患者有疼痛感,但未有发烧、发冷或其他症状。体格检查发现前额、眼睑、鼻子和面颊紫罗兰色肿胀伴毛细血管扩张和坏死,主要累及左侧面部(图1)。对皮损进行活检和组织病理学分析(图2)。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#扩张#
39
#紫罗兰色#
36
#血管扩张#
43
#毛细血管#
50
#女性患者#
30
#坏死#
29
#毛细血管扩张#
22