Lancet子刊:多发性硬化新药——赛诺菲特利氟胺对儿童也安全可靠!
2021-12-01 MedSci原创 MedSci原创
特立氟胺可能通过减少局灶性炎症活动的风险对复发性多发性硬化症儿童产生有益的影响。
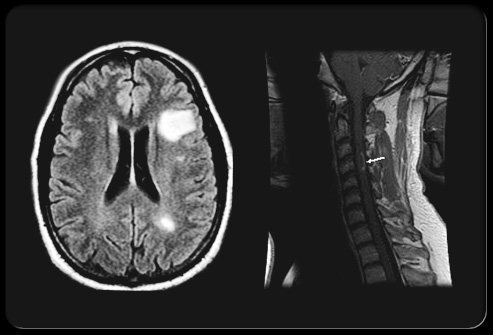
多发性硬化(multiple sclerosis,MS)是以中枢神经系统白质炎性脱髓鞘病变为主要特点的自身免疫病。本病最常累及的部位为脑室周围白质、视神经、脊髓、脑干和小脑,主要临床特点为中枢神经系统白质散在分布的多病灶与病程中呈现的缓解复发,症状和体征的空间多发性和病程的时间多发性。
本病起病年龄多在20~40岁,10岁以下和50岁以上患者少见,男女患病之比约为1∶2。其中,儿童MS患者的治疗选择很少。特立氟胺在80多个国家被批准用于治疗复发性MS的成人患者。
为了考察特立氟胺在复发性MS儿童患者中的安全性和有效性。来自麻省总院的专家开展了一项名为TERIKIDS试验——多中心、3期、双盲、平行组、随机、安慰剂对照的研究,在亚洲、欧洲、中东、北非和北美22个国家的57个临床中心进行。
该试验招募了10-17岁的复发性MS患者,在筛查前一年至少有一次复发或在筛查前两年至少有两次复发。患者被随机分配(2:1)到口服特立氟胺或匹配的安慰剂,时间长达96周。主要终点是到双盲期结束时首次确认临床复发的时间。关键的次要影像学终点是新的或扩大的T2病变的数量和每次MRI扫描的钆增强病变的数量。
从2014年7月24日到2019年10月25日期间,185名病人被筛选为合格者,166人(90%)被录取,109人被随机分配到特立氟胺,57人被随机分配到安慰剂。109人中的102人(94%)和57人中的53人(93%)完成了双盲期。在安慰剂组中,由于病灶活动而转入正在进行的开放标签扩展期的情况比预期的要多(特立氟胺组109名患者中的14名[13%]与安慰剂组57名患者中的15名[26%]),降低了研究的力量。
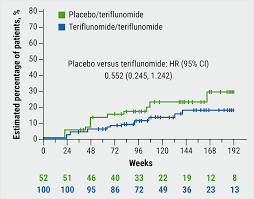
随访期间两组患者的病灶差异
96周后,特立氟胺与安慰剂相比,首次确认临床复发的时间没有差异(RR=0.66,95%CI039-1.11)。但与安慰剂相比,特立氟胺组患者新的或扩大的T2病变的数量减少了55%(RR=0.45,95%CI 029-0.71),钆增强病变的数量减少了75%(RR=0.25,0.13-0.51)。特立氟胺有96名(88%)患者发生不良事件,安慰剂组有47名(82%)患者发生不良事件。
综上,二次成像分析和对复发概率或高活动度的预先指定的敏感性分析表明,特立氟胺可能通过减少局灶性炎症活动的风险对复发性多发性硬化症儿童产生有益的影响。
参考文献:
Safety and efficacy of teriflunomide in paediatric multiple sclerosis (TERIKIDS): a multicentre, double-blind, phase 3, randomised, placebo-controlled trial. https://doi.org/10.1016/S1474-4422(21)00364-1
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言


















#Lancet#
34
#多发性#
37
谢谢
61
学习已读已读已读已读已读已读已读已读已读已读已读已读已读已读已读
68
学习了
59