Ann Rheum Dis:JIA儿童接受TNF抑制剂治疗会增加银屑病发病率
2022-02-19 MedSci原创 MedSci原创
在大型前瞻性的JIA患者队列中,研究人员观察到接受TNFi治疗后银屑病风险增加近三倍。
肿瘤坏死因子抑制剂(TNFi)已被批准用于治疗儿童幼年特发性关节炎(JIA)。伴有基础疾病(包括JIA、炎症性肠病(IBD)和慢性非细菌性骨髓炎(CNO))的儿童在接受TNFi治疗后可能会发展为银屑病。最常见的儿科症状包括斑块和掌跖脓疱型银屑病,其解剖分布与使用TNFi无关的银屑病病变相似。

近日,风湿病领域顶级期刊Annals of the Rheumatic Diseases上发表了一篇研究文章,研究人员使用儿童关节炎和风湿病研究联盟(CARRA)登记数据旨在探究肿瘤坏死因子抑制剂(TNFi)治疗与幼年特发性关节炎(JIA)儿童新发银屑病之间的关系。

研究人员从CARRA登记处获得患者的数据。在JIA诊断日期或之前记录的炎症性肠病或银屑病患者或数据不完整的患者被排除在外。根据接受TNFi治疗情况分为:(1)曾经使用过;(2)当前使用或(3)仅限首次使用。根据甲氨蝶呤治疗情况、性别、种族、银屑病家族史和初始JIA类别调整了治疗组和未治疗组之间的调整后风险比(aHR)。
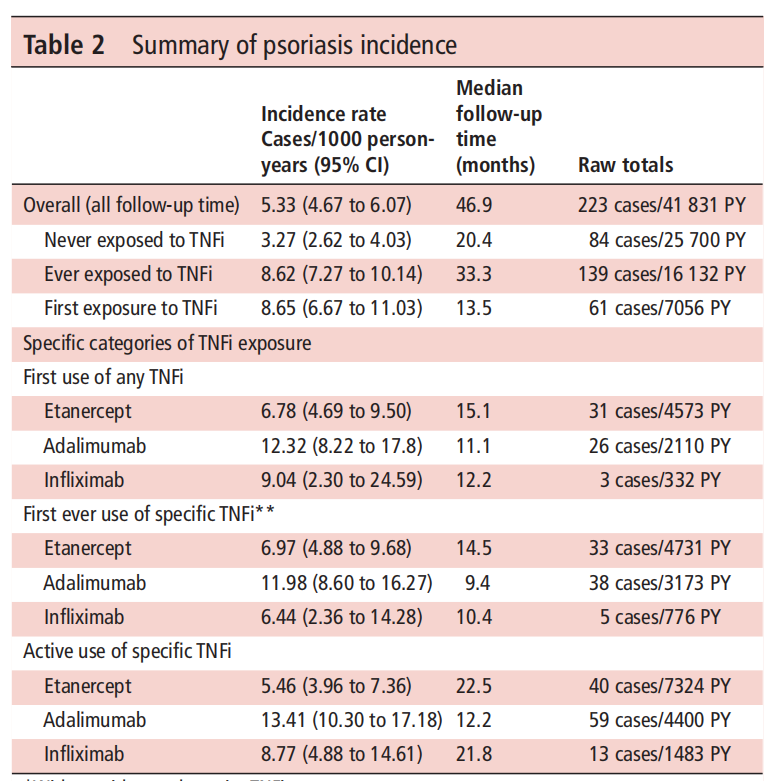
该研究共纳入了8225例患者,中位随访时间为3.9年。超过一半的患者接受了TNFi治疗(n=4437,54%)。接触TNFi治疗后新发银屑病的aHR为2.93(2.15至3.98)。在既往接受和积极接受阿达木单抗治疗的儿童中,银屑病的发病率最高。曾经同时使用甲氨蝶呤(HR为0.45,0.29至0.69)与较低的风险相关。
由此可见,在大型前瞻性的JIA患者队列中,研究人员观察到接受TNFi治疗后银屑病风险增加近三倍。
原始出处:
Yongdong Zhao,et al.Psoriasis rate is increased by the exposure to TNF inhibition in children with JIA.Ann Rheum Dis.2022.https://ard.bmj.com/content/early/2022/01/26/annrheumdis-2021-221694
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#抑制剂#
38
#Dis#
41
#发病率#
35
?
53
#TNF#
46
#JIA#
48
学习一下
61
学习
51