2021原发性胆汁性胆管炎诊疗规范,来看看指南!
2022-02-22 small year MedSci原创
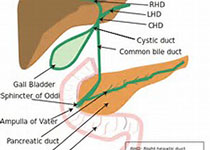
原发性胆汁性胆管炎(PBC)是一种以肝脏小胆管为主要靶器官的慢性进展性自身免疫性胆汁淤积性疾病,其主要病理改变为肝内小胆管非化脓性炎症,最终导致肝纤维化及肝硬化。
原发性胆汁性胆管炎(PBC)是一种以肝脏小胆管为主要靶器官的慢性进展性自身免疫性胆汁淤积性疾病,其主要病理改变为肝内小胆管非化脓性炎症,最终导致肝纤维化及肝硬化。
在我国 PBC 并非罕见,但规范化的诊断和治疗水平仍有待提升,在结合我国临床实践的基础上制订原发性胆汁性胆管炎诊疗规范,对规范我国PBC的临床诊断与治疗有着重要意义。本文将《2021原发性胆汁性胆管炎诊疗规范》核心要点进行整理,包括PBC的临床特点、治疗选择及预后判断,为临床医师提供指导与决策依据。
一、PBC的临床特点
随着对PBC的认识及临床诊断水平的提高,我国PBC患病率呈上升趋势。据数据显示,2010年我国PBC的患病率为 49.2/10 万,其中 40 岁以上女性的患病率为 155.8/10 万。
在早期,绝大多数PBC患者无明显临床症状,部分出现瘙痒、乏力等症状。然而,随着病程进展,PBC患者可出现皮肤和巩膜黄染、纳差、恶心等胆汁淤积及门静脉高压相关临床表现,部分合并口干、眼干、骨质疏松及其他自 身免疫病相关表现。PBC的自然史大致分为四个阶段:
临床前期:此阶段可能仅血清中高滴度抗线粒体抗体 (AMA)等自身抗体阳性,无血清生物化学指标异常,该阶段通常在10年以上。
无症状期:该阶段表现为生物化学指标异常,无明显临床症状,该阶段约5~10年。
症状期:此阶段出现乏力、瘙痒等临床表 现,从症状出现至进展为肝硬化的时间约5~8年。
失代偿期:该阶段出现门静脉高压等肝硬 化失代偿表现,生存期可能小于3年。
PBC常见的并发症包括胆汁淤积相关和肝外脏器受累,合并疾病涉及自身免疫病以及肝脏恶性肿瘤,据研究显示,PBC患者发生肝细胞肉瘤的风险显著高于健康人群,尤其出现肝硬化的PBC患者患肝细胞肉瘤的风险升高了18倍。
二、PBC的诊断
在诊断过程中,PBC需要与药物性胆汁淤积、酒精性 肝硬化、梗阻性胆汁淤积、结节病、AIH、PSC 等疾 病鉴别,同时筛查有无合并其他系统性结缔组织 病或器官特异性自身免疫病,如 SS、SSc、炎症性肠病等。
下述3条满足2条,可诊断为PBC:
1、碱性磷酸酶(ALP)升高等反映胆汁淤积的血清生物化学证据。
2、血清 血清中高滴度抗线粒体抗体 (AMA)/AMA-M2 或 抗 sp100 抗 体 、抗 gp210抗体阳性。
3、肝脏组织病理学提示非化脓性破坏性胆管炎和小叶间胆管破坏等改变。
三、PBC的治疗
目前,PBC的临床药物治疗仍以熊去氧胆酸(UDCA)为主,对UDCA治疗反应欠佳者, 二线治疗可选择的有效药物较少,预后较差。
1、PBC的基础治疗
UDCA 是治疗 PBC 的一线用药,其作用机制包括利胆、细胞保护、抗炎、免疫调节等,具有改善患者生化指标、缓解病理改变和延缓病程进展的作用。
值得注意的是,UDCA 剂量选择非常重要,13~15 mg/kg 优于 5~7 mg/kg 小剂量,也优于 23~ 25 mg/kg 大剂量,如患者同时还服用消胆胺等胆汁酸螯合剂,需提前 1 小时或延后4 小时服用,以免影响UDCA药效。
对肝功能异常和肾功能不全的 PBC患者,无需调整 UDCA 的剂量。 UDCA 主要不良反应包括腹泻、胃肠道反应、皮肤瘙痒等,但发生率较低。UDCA 应长期服用,停 药可能导致生化指标反弹甚至疾病进展。
2、二线治疗
对 UDCA治疗反应欠佳的 PBC患者,目前 FDA 批准的二线治疗药物仅有 6-乙基鹅 去氧胆酸——奥贝胆酸 ,这是一种法尼酯 X受体 激动剂,目前国内正在进行临床试验。
另外,近年来发现贝特类降脂药如非诺贝特、 苯扎贝特等,有改善UDCA治疗反应不佳的PBC患者生化指标的疗效。 苯扎贝特已在临床中开始尝试使用,但需警惕转氨酶升高和 肌酐升高等可能的不良反应。由于药品说明书尚未更新,目前未将 PBC 列入适应证,正式使用还需 等待药品说明书更新。
3、对症治疗
瘙痒是PBC最突出的症状,针对瘙痒的主要药物是消胆胺和利福平。消胆胺抑制胆汁酸在肠道的重吸收,推荐剂量为4~16 g/d,与 UDCA等药物服用时的时间间隔需至少4 小时。消胆胺不耐受或疗效不佳的PBC患者,可使用利福平作为二线治疗,推荐剂量为150 mg每日2次,疗效欠佳者可逐 渐加量至600 mg/d,使用过程中需密切监测肝功能。
4、肝移植
如患者出现顽固性腹水、自发性腹 膜炎、反复食管胃底静脉曲张破裂出血、肝性脑病、 肝细胞癌等预计存活时间少于1年的情况,可考虑 肝移植。欧洲肝病学会建议,总胆红素水平达到 60 mg/L,Mayo 评分达到 7.8 分,终末期肝病模型评 分>14分时应行肝移植评估。
四、PBC的随诊评估管理
PBC是一种慢性疾病,需长 期随诊,医患配合。初次诊断后,给予UDCA治疗, 一般推荐1个月后复诊,之后可每3个月复诊1次。 6~12个月如判断患者对UDCA治疗反应欠佳,则加用二线治疗,之后可每1~3个月复查1次,评估生化 指标应答情况及对药物的耐受情况,调整治疗,直 至达到生化指标缓解;如对 UDCA 治疗反应良好, 则可改为每3~6个月复查1次。
随诊过程中,除评价生化指标外,还需关注患者心理状况,可通过瘙痒或乏力的视觉模拟评分等 量表评估。另外,还应定期检查患者肝脏超声影像 学改变、骨密度等骨质疏松相关指标、血脂情况、评估心血管事件风险、评估甲胎蛋白等肝脏恶性肿瘤 发生风险、食管静脉曲张等门静脉高压情况,综合评估患者的生活质量及病情进展情况。
参考资料:
张奉春, 王立, 帅宗文,等. 原发性胆汁性胆管炎诊疗规范(2021)[J]. 中华内科杂志, 2021, 60(8):7.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#胆汁性#
46
#原发性#
33
AMA要达到多高的滴度才有意义呢
59
#原发性胆汁性胆管炎#
45
#胆汁#
49
#胆管#
70
学习了
63
学习了
59
学习学习
0
学习
0