Nature Microbiology:病毒研究领域新突破
2019-04-16 胖胖同学 iNature
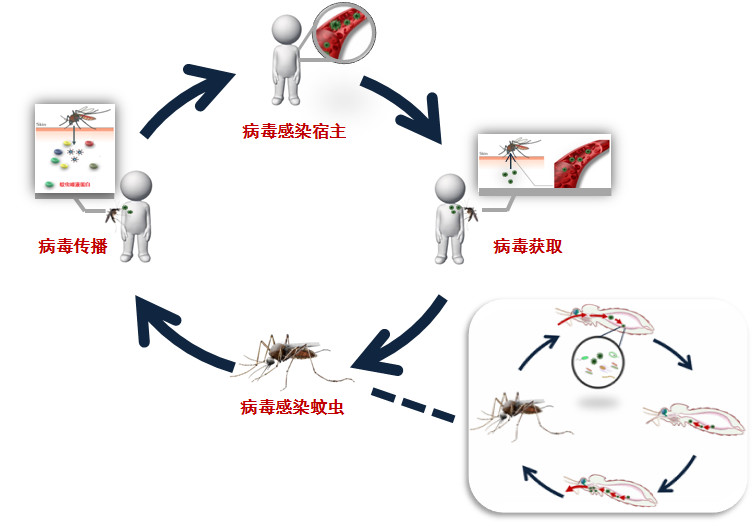
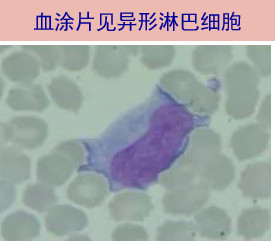
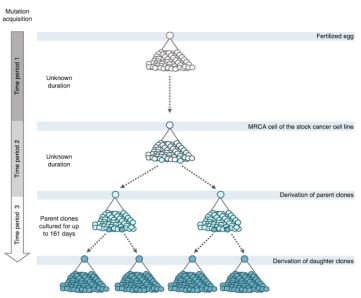
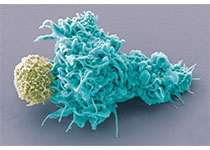
病毒感染的爆发是健康的重要威胁。虽然Ⅰ型干扰素(IFN-Ⅰ)具有广谱的抗病毒作用,但其对宿主细胞的抗病毒作用很大程度上受到病毒的限制。如何提高IFN-Ⅰ的抗病毒效果还有待进一步探讨。2019年4月15号,苏州大学郑慧、熊思东、董春升研究团队等人在Nature microbiology上在线发表了题为ADP-ribosyltransferase PARP11 modulates the interf
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#CRO#
37
#Bio#
0
#Micro#
43
#新突破#
54
#Biol#
46
#Nat#
39