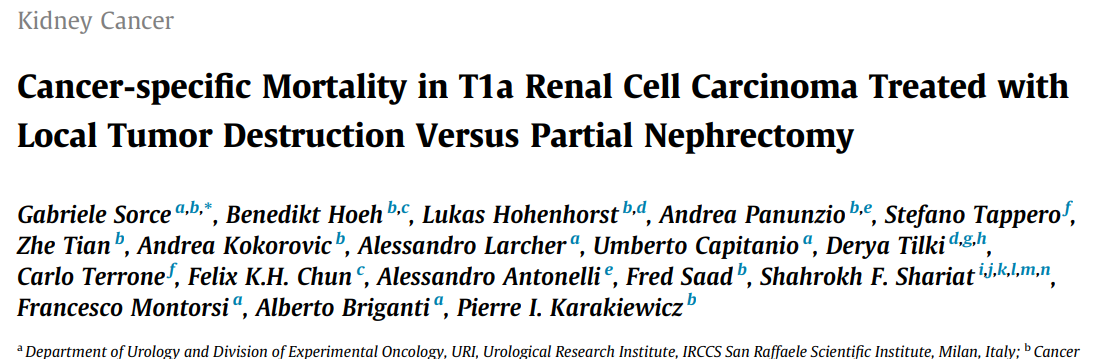
Eur Urol Focus:局部肿瘤破坏与肾部分切除术治疗T1a肾细胞癌的癌症特异性死亡率比较
2022-08-25 AlexYang MedSci原创
比较了LTD与PN后的CSM情况。
在T1a肾细胞癌(RCC)患者的癌症特异性死亡率(CSM)大规模分析中,相对于肾脏部分切除术(PN),局部肿瘤破坏(LTD)的大规模分析非常少。

近期,来自意大利的研究人员在《Eur Urol Focus》上发表文章,比较了LTD与PN后的CSM情况。
研究人员在SEER数据库中(2004-2018年)确定了使用LTD或PN治疗的临床T1a期RCC患者,并在接受LTD与PN治疗的患者之间进行了1:1比例的倾向性评分匹配(PSM)。在调整了其他原因死亡率(OCM)和其他协变量(年龄、肿瘤大小、肿瘤等级和组织学亚型)后,使用了竞争风险回归(CRR)模型来调查CSM。
与35984名PN患者相比,5936名LTD患者的年龄较大,且存在更多的未知RCC组织学亚型或等级。经过1:1的PSM,5352名LTD患者与5352名PN患者相比,10年的CSM率分别为8.7%与5.5%。在多变量CRR模型中,相对于PN,LTD与较高的CSM有关(危险比[HR]:1.58,P<0.001)。亚组分析显示,在肿瘤大小≤3厘米(10年CSM 7.2% vs 5.3%,多变量HR:1.47,p<0.001)和肿瘤大小3.1-4厘米(10年CSM 11.4% vs 6.1%,多变量HR:1.72,p<0.001)的患者中,LTD的CSM总是比PN更高。研究的主要限制是缺乏有关早期癌症控制、再治疗、肾脏内肿瘤位置和手术类型信息。
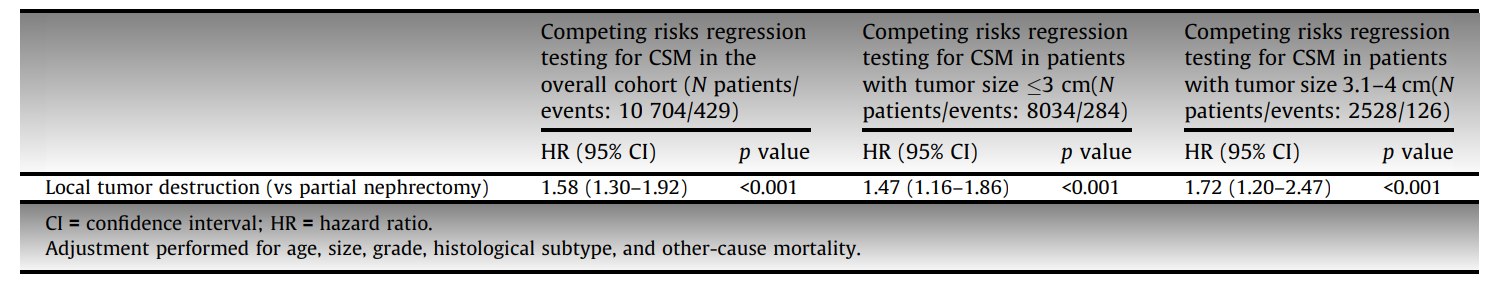
调整后癌症特异性生存情况
综上所述,在T1a RCC患者中,在调整了OCM和所有可用的患者和肿瘤特征,并且不考虑肿瘤大小时,LTD相对于PN,总有较高的CSM。并且,肿瘤大小为3.1-4厘米时,LTD患者的CSM劣势比肿瘤大小≤3厘米时更为明显。
原始出处:
Gabriele Sorce , Benedikt Hoeh , Lukas Hohenhorst et al. Cancer-specific Mortality in T1a Renal Cell Carcinoma Treated with Local Tumor Destruction Versus Partial Nephrectomy. Eur Urol Focus. Jul 2022.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#切除术#
60
#特异性#
84
#细胞癌#
58
#局部#
58
👀
0