Lancet oncol:基因突变所导致肿瘤特异性抗原和免疫表型
2017-07-08 qinqiyun MedSci原创
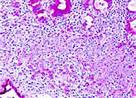
既往对于肿瘤特异性抗原的研究都集中于单核苷酸突变(SNVs),对于小片段的插入和缺失(indels)未予以明显关注。Samra Turajlic及其同事对于插入导致的移码改变进行研究,移码改变会产生新的开放阅读框和突变多肽的特性极大的改变,可能因此而产生新的免疫表型。
既往对于肿瘤特异性抗原的研究都集中于单核苷酸突变(SNVs),对于小片段的插入和缺失(indels)未予以明显关注。Samra Turajlic及其同事对于插入导致的移码改变进行研究,移码改变会产生新的开放阅读框和突变多肽的特性极大的改变,可能因此而产生新的免疫表型。
通过对来自5777例实体瘤的外显子序列进行分析,根据癌症基因组集将其分为19个癌症类型。通过对两个独立的数据库进行检索,比较各个队列间插入和缺失的数量和比例。根据突变类型评估基因芯片中肿瘤特异性抗原预测情况,以及结合肾透明细胞癌(n=392)中RNAseq,来比较患者亚群中免疫基因表达情况。通过4个检查点抑制剂的数据库来评估插入和缺失负荷和治疗反应之间的关系。
通过pan-cancer分析发现肾透明细胞癌中插入和缺失突变的比例(0.12)和数量最高,超过其他所有检测的癌症类型中插入和缺失突变的比例的中位数的两倍。对肿瘤特异性抗原的分析发现高亲和性绑定的插入和缺失突变有富集倾向,是非同义SNV突变的三倍。而且,与非同义SNV突变所产生的抗原相比,由插入缺失突变所产生的抗原会九倍富集于突变特异性结合。
对肾透明细胞癌队列进行免疫基因表达分析发现突变特异性抗原与抗原表达基因上调相关,抗原表达基因又与CD8阳性的T细胞活化相关。最后,对检查点抑制剂数据的分析表明在三个分开的黑色素瘤队列中移码插入缺失与检查点抑制剂表达高度相关。
肾透明细胞癌有最高的插入缺失突变的pan-cancer比例和数量。证据表明插入和缺失是一种高度免疫性突变类型,其可以触发大量抗原的上调和增加突变结合特异性。
原始出处:
Samra Turajlic,Kevin Litchfield,et al.Insertion-and-deletion-derived tumour-specific neoantigens and the immunogenic phenotype: a pan-cancer analysis. The Lancet Oncology.7 July 2017.http://dx.doi.org/10.1016/S1470-2045(17)30516-8
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#Oncol#
23
#特异性抗原#
32
#特异性#
26
#Lancet#
30
基因突变所导致肿瘤特异性抗原。
44
#表型#
18
#抗原#
22