IJLH:细胞凋亡可以作为儿童急性髓系白血病高风险表型的生物标志物?
2019-06-02 不详 网络
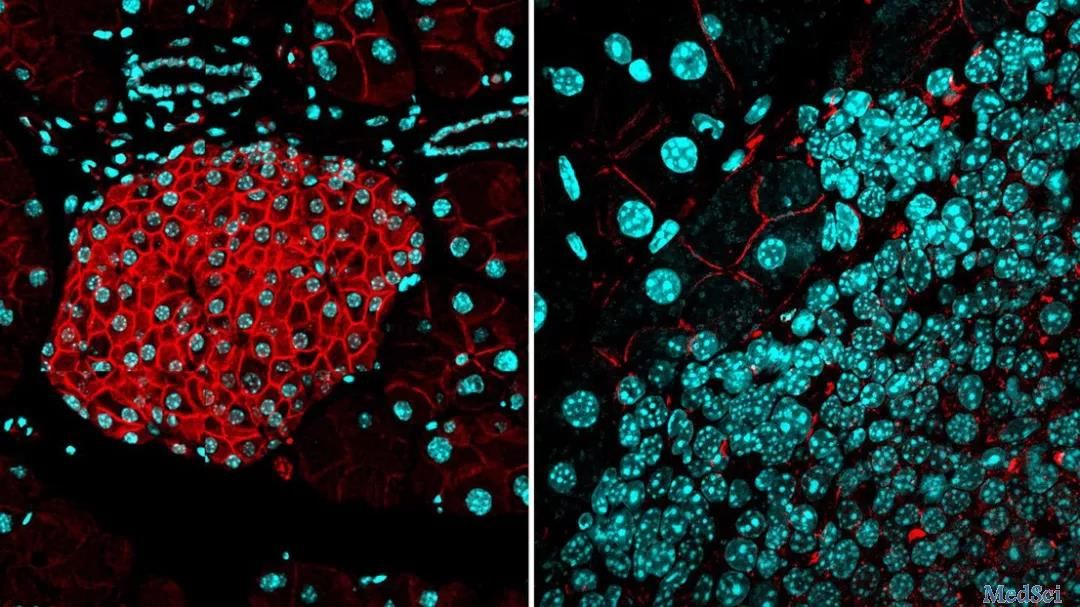
已经有研究在急性髓性白血病(AML)中探索了细胞凋亡的调节异常;然而,它与儿科AML临床结果的相关性尚不清楚。本研究旨在分析儿童AML患者通过内在途径介导的细胞凋亡和凋亡百分比以及临床结果。 本前瞻性研究纳入2013年7月至2016年8月登记的儿童AML患者。流式细胞仪检测基线骨髓(BM)中Annexin‐V(总凋亡标志物)和caspase‐9(内在通路标志物)的表达,并与对照组(未受实体瘤
已经有研究在急性髓性白血病(AML)中探索了细胞凋亡的调节异常;然而,它与儿科AML临床结果的相关性尚不清楚。本研究旨在分析儿童AML患者通过内在途径介导的细胞凋亡和凋亡百分比以及临床结果。
本前瞻性研究纳入2013年7月至2016年8月登记的儿童AML患者。流式细胞仪检测基线骨髓(BM)中Annexin‐V(总凋亡标志物)和caspase‐9(内在通路标志物)的表达,并与对照组(未受实体瘤影响的BM和未受影响的同胞外周血[PB]进行比较。使用log‐rank测试比较总体生存期(OS)和无事件生存期(EFS)。
本研究共纳入151例AML患者,中位年龄10岁(范围:0.7‐18岁)。AML患者中Annexin‐V的表达明显高于实体瘤患者的BM (P = 0.01)和健康患者的PB (P = 0.04)。Caspase‐9在胚细胞中的表达无显著差异。在WBC计数≥11000 /mm3 (P = 0.02)、‐细胞遗传学不良(P = 0.02)、RUNX1‐RUNX1T1易位缺失(P = 0.004)和NPM1突变缺失(P = 0.05)的患者中,annexin‐V的中位表达显著增高。高annexin‐V表达的患者在单因素分析中OS明显低于对照组(P = 0.05),而在多因素分析中则无差异(P = 0.32)。
研究表明,急性髓系白血病(AML)基线BM标本中细胞凋亡总体呈激活状态。在该疾病中,高凋亡可能与高风险表型有关。
原始出处:
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#髓系白血病#
20
#高风险#
23
#标志物#
31
#细胞凋亡#
27
#表型#
22
#生物标志#
23
#生物标志#
24