JCO:多发性骨髓瘤的自体移植,巩固和维持治疗
2019-01-19 海北 MedSci原创
最近,研究人员设计了一项前瞻性,随机,III期研究,通过比较AHCT,串联AHCT(AHCT / AHCT),AHCT以及随后的4个len,bortezomib和地塞米松(RVD; AHCT + RVD)周期,测试其他干预措施以改善PFS。
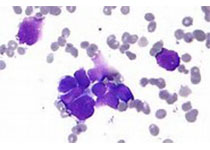
单循环马法兰200 mg/m2和自体造血细胞移植(AHCT)以及来那度胺(len)维持治疗可改善符合移植标准的多发性骨髓瘤(MM)患者的无进展生存期(PFS)和总生存期(OS)。
最近,研究人员设计了一项前瞻性,随机,III期研究,通过比较AHCT,串联AHCT(AHCT / AHCT),AHCT以及随后的4个len,bortezomib和地塞米松(RVD; AHCT + RVD)周期,测试其他干预措施以改善PFS。
在开始治疗后12个月内有症状,且70岁或以下无进展的MM患者被随机分配到AHCT / AHCT + len(n = 247),AHCT + RVD + len(n = 254)或AHCT + len (n = 257)组。该实验的主要终点是38个月的PFS。
研究人群的中位年龄为56岁(范围为20至70岁); 24%的患者患有高风险MM,73%的患者采用三联药物治疗作为初始治疗,18%的患者在入组时具有完全反应。
AHCT / AHCT + len的38个月PFS率为58.5%(95%CI,51.7%至64.6%),AHCT + RVD + len为57.8%(95%CI,51.4%至63.7%),AHCT + len为53.9% (95%CI,47.4%至60%)。对于AHCT / AHCT + len,AHCT + RVD + len和AHCT + len,OS率为81.8%(95%CI,76.2%至86.2%),85.4%(95%CI,80.4%至89.3%),和83.7%(95%CI,78.4%至87.8%),1年的完整反应率分别为50.5%(n = 192),58.4%(n = 209)和47.1%(n = 208)。各治疗组的毒性特征和第二原发性恶性肿瘤的发展相似。
因此,第二次AHCT或RVD合并作为AHCT后干预措施,对符合移植标准的MM患者进行前期治疗并未改善PFS或OS。单个AHCT和len应该仍然是该人群的标准疗法。
原始出处:
Stadtmauer EA et al. Autologous Transplantation, Consolidation, and Maintenance Therapy in Multiple Myeloma. JCO, 2019; doi: 10.1200/JCO.18.00685.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#JCO#
26
#多发性#
27
#自体移植#
30
学习了,谢谢作者分享!
0