Liver Int:肝硬化门脉高压患者中循环的CXCL10可能能够反映全身炎症,并能够预测ACLF和死亡率
2018-05-14 MedSci MedSci原创
循环的CXCL10可能反映全身炎症,与急性失代偿、ACLF和严重门静脉高压症患者的并发症相关。CXCL10预测这些患者的生存率和CXCL10的减少可能被认为是一个好的预后因素。
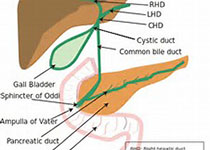
研究背景和目的:CXCL9和CXCL11与接受肝内肝静脉系统分流(TIPS)的患者的生存率有关;然而,目前对CXCL10在门脉高压中发挥的作用,并不清楚。
研究方法:本研究纳入89例肝硬化患者。在进行TIPS介入时和实行介入后2周,测量24例患者门静脉和肝静脉血液中CXCL10蛋白水平。在实行TIPS介入时,在另外25名患者中的门静脉、肝静脉、肘静脉和右心房血液中,分别评估CXCL10和IL8水平。在40例患者中,采用实时PCR法,检测CXCL10 mRNA水平。
研究结果:肝脏CXCL10水平与肝硬化失代偿没有相关性。相比之下,在门静脉内,循环CXCL10水平高于肝静脉血液的水平,提示肝硬化中CXCL10的肝外来源。然而,来自门静脉、肝静脉、肘静脉和右心房中的CXCL10蛋白水平,彼此相关,且与IL-8水平有显著相关性。较高的CXCL10循环水平与腹水的存在和较高的Child评分有关。较高的CXCL10循环蛋白水平与急性失代偿、慢加急性肝衰竭(ACLF)和死亡率相关。此外,实施TIPS后,CXCL10蛋白水平的降低与每个队列中较好的存活率有关。
研究结论:循环的CXCL10可能反映全身炎症,与急性失代偿、ACLF和严重门静脉高压症患者的并发症相关。CXCL10预测这些患者的生存率和CXCL10的减少可能被认为是一个好的预后因素。
原始出处:
Lehmann JM, Claus K, Jansen C, et al. Circulating CXCL10 in cirrhotic portal hypertension might reflect systemic inflammation and predict ACLF and mortality. Liver Int, 2018, 38(5), 875-884.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#ACLF#
40
#CXCL1#
48
#CXCL10#
57
#门脉高压#
48
#全身炎症#
43
不错的文章值得推荐
45