
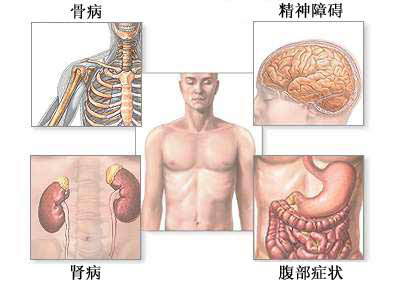
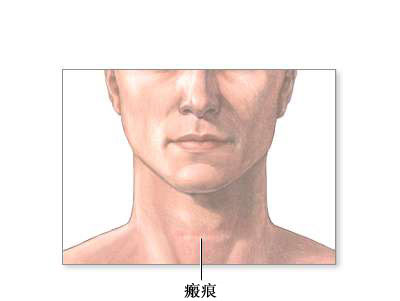
甲状旁腺切除术适用于甲状旁腺功能亢进:甲状旁腺分泌过多的甲状旁腺激素,导致血钙增高,引起一系列症状:肌肉痉挛或抽搐、骨质脆弱(骨质疏松症)、肾病(包括肾结石)、精神问题(情绪低落、易怒、疲乏、焦虑),以及腹痛、恶心、呕吐等。但是,许多患者没有任何症状。常规血液检查可以发现血钙增高。
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#切除术#
33
#适应症#
27
#甲状旁腺#
29
#甲状旁腺切除术#
35