AM J CARDIOL:压力是冠心病的危险因素,与性别无关
2017-06-15 MedSci MedSci原创
压力,尤其是女性的压力,正越来越多地被认为是冠心病的主要危险因素,冠心病是由于炎症、栓塞等导致冠状动脉血管管腔狭窄或闭塞引起的心脏病。在一项新的研究中,加州大学洛杉矶分校的研究人员推测,简单的生物标志物--尿液中的应激激素多巴胺、肾上腺素、去甲肾上腺素和肾上腺皮质激素--与冠状动脉中的钙离子浓度有关,这些生物标志物提示冠心病的存在,且这种作用在女性中的表现强于男性。然而,研究人员发现,实际上这种关
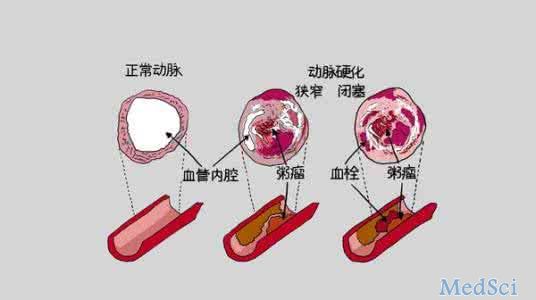
压力,尤其是女性的压力,正越来越多地被认为是冠心病的主要危险因素,冠心病是由于炎症、栓塞等导致冠状动脉血管管腔狭窄或闭塞引起的心脏病。
在一项新的研究中,加州大学洛杉矶分校的研究人员推测,简单的生物标志物--尿液中的应激激素多巴胺、肾上腺素、去甲肾上腺素和肾上腺皮质激素--与冠状动脉中的钙离子浓度有关,这些生物标志物提示冠心病的存在,且这种作用在女性中的表现强于男性。
然而,研究人员发现,实际上这种关系在男女之中是相似的: 尽管女性的尿液中的应激激素水平平均高于男性,但在两种性别中,冠状动脉钙化所测量的压力与无症状冠心病之间的联系是相似的。特别是,尿液中的皮质醇是无症状冠心病的一种强大独立预测因子。
研究人员也惊讶地发现,一种应激激素多巴胺与心脏病风险呈负相关。他们发现,高水平的多巴胺与降低冠状动脉钙的几率有关。
研究人员说,总的来说,这是第一个证明尿液中的应激激素与动脉中实际积累的斑块相关的研究。
心脏病是导致美国人死亡的主要原因,所以预防心脏病是很重要的。越来越多的研究认为压力是冠心病的主要危险因素。先前的研究表明,应激激素--尿液中的儿茶素(多巴胺、肾上腺素和去甲肾上腺素)和皮质醇(皮质激素)与心理压力、抑郁和焦虑有关。以前的研究没有研究尿液中的应激激素和冠状动脉钙化之间的关系,尽管之前的研究发现在动脉中有唾液皮质醇和血小板聚集之间存在关联。
654名参与者(53%的女性)参与了这项大规模的、正在进行的以人群为基础的心血管危险因素的调查,这项研究被称为对动脉粥样硬化的多民族研究。研究人员收集一份参与者12小时的尿液,并分析其应激激素的水平。还通过计算机断层扫描(CT)扫描受试者的胸部,以确定他们冠状动脉中可见的钙含量,并计算他们的冠状动脉钙化指数。
研究人员下一步是研究尿液中应激激素和心血管疾病(如心脏病发作或中风)之间的关系。
通过简单的尿检来量化压力水平,这个简单的测试有助于冠心病的预测,同时这项工作可以为冠心病和心脏病提供新的预防策略。
原文出处: Rachel T. Zipursky et al. Relation of Stress Hormones (Urinary Catecholamines/Cortisol) to Coronary Artery Calcium in Men Versus Women (from the Multi-Ethnic Study of Atherosclerosis [MESA]), The American Journal of Cardiology (2017).
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#Cardiol#
34
学习了谢谢分享。
0
学习了谢谢分享。
60
学习了分享了
67
个体因素
80
我觉得不靠谱
60