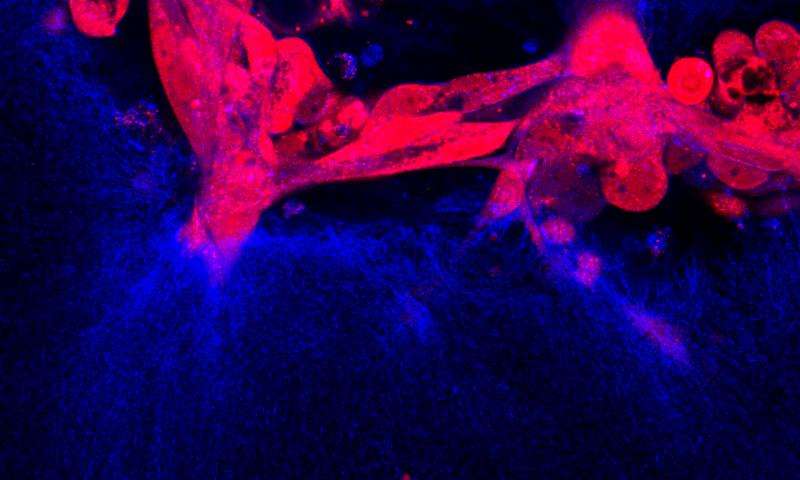
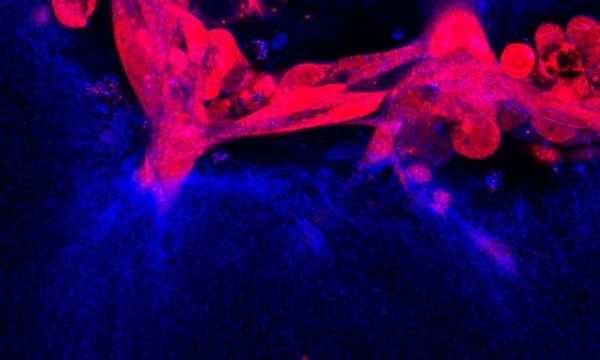
Oncogene:卵巢癌是如何扩散的?
2017-06-28 枫丹白露 来宝网
每年有20,000次诊断,卵巢癌是美国妇女中第九大常见癌症和癌症死亡的第五大原因。这么多的女性因卵巢癌而死亡,因为它常常在骨盆和腹部扩散之前才被检出,至此难以治疗,通常是致命的。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Gene#
27
新的转移机制,必然带来新的治疗方式,学习了!
73
#Oncogene#
34
学习了。。。。
75
学习了,谢谢分享
60
好文章学习了
74
学习了,谢谢作者分享!
70