Acta Neuropathologica: 松果体实质肿瘤的临床和分子异质性:一项共识性研究
2021-04-27 MedSci原创 MedSci原创
松果体实质肿瘤是一种罕见的中枢神经系统(CNS)肿瘤,包括一系列具有不同组织学表现和临床表型的实体。松果体实质性肿瘤占所有CNS肿瘤的< 1%。
松果体实质肿瘤是一种罕见的中枢神经系统(CNS)肿瘤,包括一系列具有不同组织学表现和临床表型的实体。松果体实质性肿瘤占所有CNS肿瘤的< 1%,包括世界卫生组织(WHO)1级松果体细胞瘤到WHO 2-3级中间分化松果体实质肿瘤(PPTIDs)以及4级松果母细胞瘤(PBs),PBs主要是胚胎肿瘤。

最近有基因组研究揭示了松果体实质肿瘤的生物学和肿瘤间异质性,特别是PBs和PPTIDs。然而,以前的报告样本量不大,缺乏整合分子和临床发现的能力。本研究对221例具有分子特征的PBs和PPTID患者进行了荟萃分析。通过互补生物信息学方法分析DNA甲基化谱并协调分子亚组。对这些松果体肿瘤患者和样本的人口统计学、临床和基因组特征进行了注释。
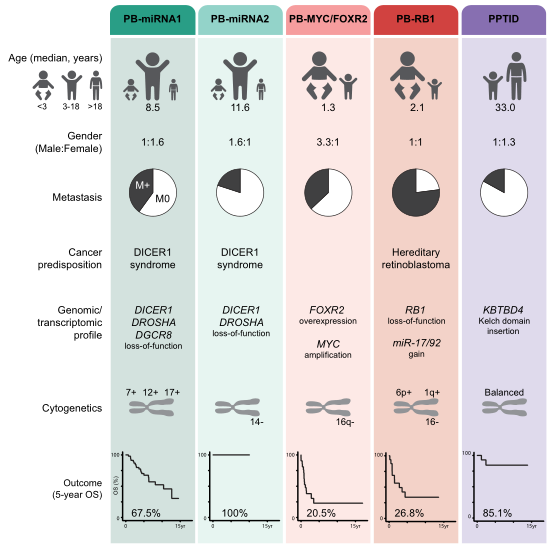
图1:松果体实质肿瘤的临床和分子特征的概述
这项研究定义了四个临床和生物学相关的共识PB组,包括PB-miRNA1(n=96)、PB-miRNA2(n=23)、PB-MYC/FOXR2(n=34)和PB-RB1(n=25)。最后一个分子独特的组,命名为PPTID(n=43),包括组织学上的PPTID和PBs。基因组学和转录组学分析允许对单个肿瘤组的致癌驱动因素进行表征,特别是PB-miRNA1/2中microRNA处理途径的改变,PB-MYC/FOXR2中MYC扩增和FOXR2过度表达,PB-RB1中RB1的改变以及PPTID中KBTBD4的插入。
研究结果显示,不同肿瘤组的诊断年龄、性别偏好和转移状况存在显著差异。尽管PB-miRNA2和PPTID患者的预后较好,但PB-miRNA1患者的生存率居中,而PB-MYC/FOXR2或PB-RB1患者的生存率较低。
综上所述,这项研究证实了松果体实质肿瘤的临床和生物学异质性,并提出了一致的分子组。未来的PB临床研究应该对患者进行分子分层,以便进行个性化管理。
原始出处:
Liu, A.P.Y., Li, B.K., Pfaff, E. et al. Clinical and molecular heterogeneity of pineal parenchymal tumors: a consensus study. Acta Neuropathol 141, 771–785 (2021). https://doi.org/10.1007/s00401-021-02284-5
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#肿瘤异质性#
56
#分子异质性#
26
#pathologic#
36
#Pathol#
39
#松果体#
34
#CTA#
29