Circulation:孕期及产后期可显著增加主动脉夹层或破裂的风险
2016-08-08 MedSci MedSci原创
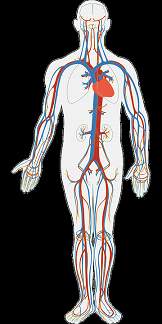
既往报道过一系列妊娠期间发生主动脉夹层和破裂的病例。但是,很少有以人口为基础的研究数据来支持二者之间的关联。 本研究进行了一项较差队列研究,2005-2013年间纳入年龄≥12岁分娩或流产女性。研究结果为主动脉夹层或破裂。根据孕期报告的主动脉并发症的时间,我们定义了风险期为分娩前6个月到分娩后3个月。我们比较了每一位病人在此期间主动脉并发症发生的可能性。使用条件泊松回归和稳健标准误来计算发病
既往报道过一系列妊娠期间发生主动脉夹层和破裂的病例。但是,很少有以人口为基础的研究数据来支持二者之间的关联。
本研究进行了一项较差队列研究,2005-2013年间纳入年龄≥12岁分娩或流产女性。研究结果为主动脉夹层或破裂。根据孕期报告的主动脉并发症的时间,我们定义了风险期为分娩前6个月到分娩后3个月。我们比较了每一位病人在此期间主动脉并发症发生的可能性。使用条件泊松回归和稳健标准误来计算发病率和发病率比。
4933697名女性中共有6566826名孕妇,36名女性在孕期或产后期发生了主动脉夹层或破裂,9名女性在对照期1年后发生。怀孕期间和产后期主动脉并发症的发生率为5.5/100万,而等效对照1年期间主动脉并发症的发生率为1.4/100万。与对照期1年相比,妊娠与主动脉夹层或破裂的风险明显增加相关。
总而言之,该研究表明,妊娠期和产后期女性主动脉夹层或破裂的风险升高。
原始出处:
Hooman Kamel, Mary J. Roman, Alex Pitcher and Richard B. Devereux. Pregnancy and the Risk of Aortic Dissection or Rupture: A Cohort-Crossover Analysis. Circulation. 2016;doi:10.1161/CIRCULATIONAHA.115.020627.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













值得学习
65
继续关注
75
继续学习
57
#主动脉#
28
#动脉夹层#
35
做母亲好伟大
67
好好学习
59
谢谢,学习了。
22
学习学习!
26