恶心呕吐是临床上最常见的症状之一,看似简单,但具体找到病因,实属不易。恶心呕吐是通过胃、食管、口腔、膈肌和腹肌等部位的协同作用,使胃内容物经食管、口腔而排出体外,是一种复杂的生理反射过程。
一、恶心呕吐病因
恶心呕吐是一种特殊的主管感受,表现为胃部不适和胀满感,通常是呕吐的前奏,多伴有流涎与反复的吞咽动作,同时严重者伴有头痛、头晕、出汗、面色苍白及心率加快等表现。
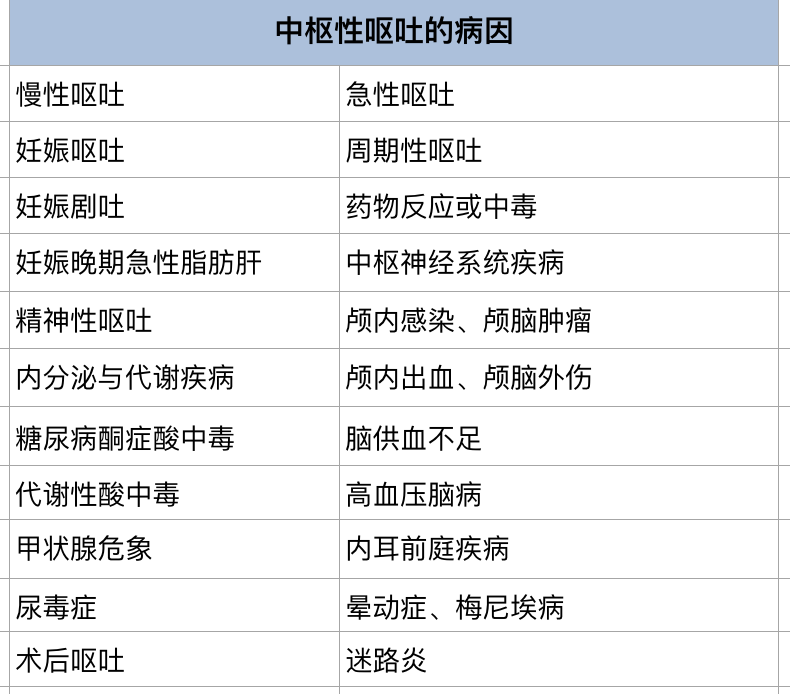
引起恶心与呕吐的病因很多,临床上通过分为反射性呕吐和中枢性呕吐。反射性呕吐常由胃肠道疾病、肝胆胰疾病、腹膜及肠系膜疾病、肾脏疾病、青光眼等引起。中枢性呕吐主要是由神经系统疾病、全身性疾病、抗癌药、吗啡等药物以及中毒及精神因素等导致。

二、恶心呕吐治疗
由于引起恶心呕吐的疾病很多,在未明确病因之前不应盲目用药。恶心呕吐的治疗原则包括病因治疗、对症治疗和纠正水电解质失衡等。
1、病因治疗
如果恶心呕吐的病因明确,治疗原发病即可得到控制。炎症引起的恶心呕吐者,应积极抗感染治疗。如果确定为胃肠道梗阻患者,应采取药物或手术治疗。各种原因引起的颅内高压者,应给予手术治疗或根据病情采取相应措施。对于精神性呕吐,应进行心理治疗,是患者树立战胜疾病的信心,同时给予镇静及调节自主神经功能失调等治疗。
2、对症治疗
恶心、呕吐的发生有多种神经递质和受体参与,患者恶心呕吐频繁,应给予对症治疗。那么,止吐药有哪些?不同疾病引起的恶心、呕吐如何选用止吐药呢?
1)抗组胺类药物
抗组胺类药物常用的H1受体阻滞剂,主要通过抑制呕吐中枢,以及作用于前庭核和网状结构的胆碱能神经元,从而抑制呕吐反射。H1受体阻滞剂主要包括异丙嗪、美可洛嗪、氯苯那敏、阿司咪唑等药物。有动物研究显示,该类药物有致畸作用,孕妇应慎用。
2)抗胆碱类药物
抗胆碱类药物种类繁多,用者有阿托品、山莨菪碱、东莨菪碱等。阿托品和山莨菪碱主要通过降低迷走神经的兴奋性,增加贲门括约肌的张力,解除胃肠痉挛,预防呕吐和反流,常常用于预防术前呕吐。而东莨菪碱为节后抗胆碱类药物,可抑制中枢神经系统,对镇静、催眠和止吐有作用,对晕动症所致恶心呕吐有良好的疗效。然而,抗胆碱类药物也有一些不良反应,比如口干,面色潮红,心率加快等。
3)促进胃肠蠕动药物
目前常用的药物有甲氧氯普胺、多潘立酮、西沙比利和红霉素等。甲氧氯普胺是普鲁卡因胺的衍生物,能阻止多巴胺受体,进而减少恶心呕吐的冲动。同时,甲氧氯普胺能促进幽门蠕动,扩张幽门管,缩短胃排空时间,还能使胃平滑肌对乙酰胆碱的敏感性增强,从而改善胃蠕动功能。
4)5-HT拮抗剂
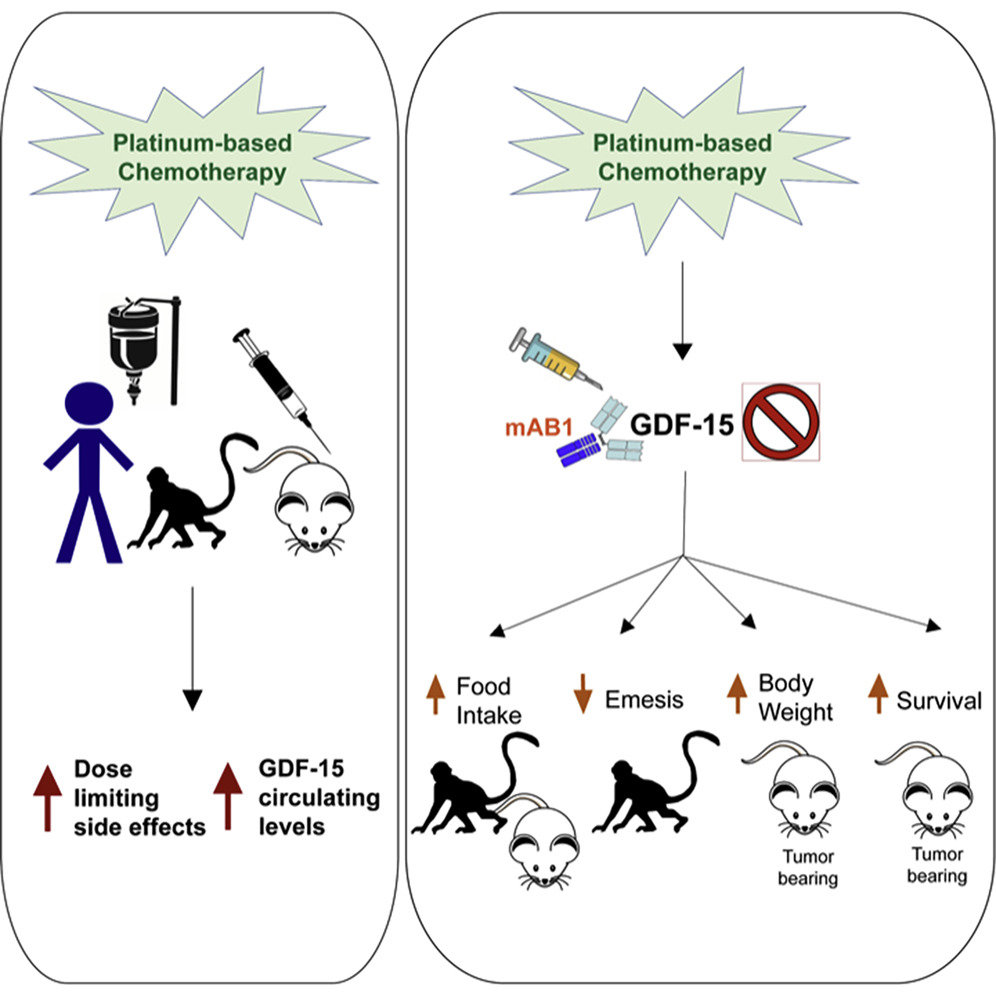
全身90%的5-HT由胃肠道黏膜嗜铬细胞分泌,其可激活肠粘膜及中枢CTZ的5-HT3受体,而5-HT3 受体拮抗剂通过选择性阻断外周和中枢的 5-HT3 受体,从而有效控制化疗引起的呕吐。
目前已合成选择性5-HT3 受体拮抗剂,并广泛应用于临床。其中,5-HT3 受体拮抗剂常用的药物有恩丹西酮,格雷司酮,托烷司琼等。5-HT3 受体拮抗剂首先用于化疗所产生的呕吐,当然对与放疗和手术后所致的呕吐也效。当患者对其他止吐药无效时,应用5-HT3 受体拮抗剂治疗。5-HT3 受体拮抗剂耐受范围广,不良反应小,通常有轻度和中度的头痛,头晕,便秘和腹泻等。
5)吩噻嗪类药物
吩噻嗪类药物主要通过选择性地抑制CTZ或(和)直降低延髓呕吐中枢的兴奋性,发挥止呕作用,常用药物包括氯丙嗪、异丙嗪、奋乃静、三氟拉嗪和丙氯拉嗪等。该类药物对某些药物(如阿片类、麻醉药和化疗药)引起的恶心呕吐效果较好,对放疗和胃肠道病变所致的心呕吐亦有效。
氯丙嗪在临床上最为常用,其止作用机制主要是抑制CTZ,也能对抗阿扑吗啡的催吐作用。术前应用氯丙嗪可减少术后恶心呕吐发声率达50%;若术后治疗性应用该药,大约30%患者的恶心呕吐症状得以控制。异丙嗪具有镇静和较强的抗组胺作用,能抑制CTZ和前庭系统。
6)丁酰苯类药物
丁酰苯类药物主要通过抑制中枢的CTZ,产生强抗呕吐作用,对预防和治疗术后恶心呕吐有良好的效果,常用药物有氟哌啶醇、氟哌利多等。肌内注射氟哌啶醇1mg,在1~5小时内,80%~100%的术后恶心呕吐得以控制。氟哌利多的抗吐作用比氟哌啶醇效果好,该药静脉注射5~8分钟起效,最佳效应持续3~6小时。然而,丁酰苯类药物常有嗜睡、焦虑不安、延迟性锥体外系反应、术后苏醒延迟、呼吸抑制及低血压等不良反应。
7)大麻碱类药物
大麻碱类药物作用机制尚不清楚,可能与精神活动有关的额叶,反射性抑制延髓呕吐中枢有关。这类常用的药物包括四氢大麻素和庚苯吡酮,主要用于化疗药物诱发恶心呕吐的止呕作用。化防前30分钟口服庚苯吡酮,抗恶心呕吐的有效达80%,其作用明显优于吩噻嗪类药物,但该类药物不良反应较大,比如困倦,口干,视物不清等。
8)NK1受体拮抗剂
P 物质 (substance P,SP)为含 11 个氨基酸的多肽, 同属于速激肽(又称神经激肽)家族,速激肽受体有 NK-1、NK-2 和 NK-3,其中 P 物质与 NK-1 的亲和力最强。 SP 有致吐作用,而选择性 NK-1 受体拮抗剂则能抑制其致吐。
NK1受体拮抗剂的主要药物有阿瑞吡坦、福沙吡坦。阿瑞吡坦是首个获批应用于临床的NK1受体拮抗剂。与5-HT3 受体拮抗剂联用,进一步减轻顺铂诱发的急性和迟发性呕吐。中国抗癌协会癌症康复与姑息治疗专业委员会发布 了 2014 年版《中国肿瘤治疗相关呕吐防治指南》,提出 预防为主的治疗原则,推荐把“三联方案”——阿瑞匹坦、 5-HT3 受体拮抗剂、联用地塞米松作为化疗止吐的一线治疗方案,此方案与美国 NCCN 指南基本一致。阿瑞匹坦的耐受性较好,常见不良反应有厌食、 虚弱、 疲 劳、 便秘、 腹泻和恶心呕吐等,发生率在10%~18%之间。
9)糖皮质激素
糖皮质激素可用于治疗化疗相关性呕吐,也用于减轻颅内压增高所致的恶心呕吐,常用药物为地塞米松。然而,糖皮质激素作用机制目前尚未明确,有研究认为可能是过抗炎及抗毒素的作用,减轻外周神经的损害,保持正常的胃肠动力,从而减轻迟发性呕吐。另外,有学者认为是通过外周和中枢两种途径抑制5-HT产生和释放起到止吐作用。
10)苯二氮䓬类药物
短效苯二氮䓬类药物常用于缓解恶心,其止吐效果较弱,首选药物为劳拉西泮。这类药物主要作用为镇静、抗焦虑,因此对与焦虑有关的恶心呕吐作用较好,还可提高其他止吐药物的疗效,也可预防呕吐。
参考资料
1.王孟军. 止吐药研发现状及发展趋势[J]. 上海医药, 2014, 35(17):6.
2.于皆平, 沈志祥, 罗和生. 实用消化病学(第2版)(精)[M]. 科学出版社, 2007.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










谢谢分享
46
总结全面
63
坚持学习
73
学习了
77
#止吐药#
46
好文章
69
学习了
74
学习!
0
学习
49
学习学习
55