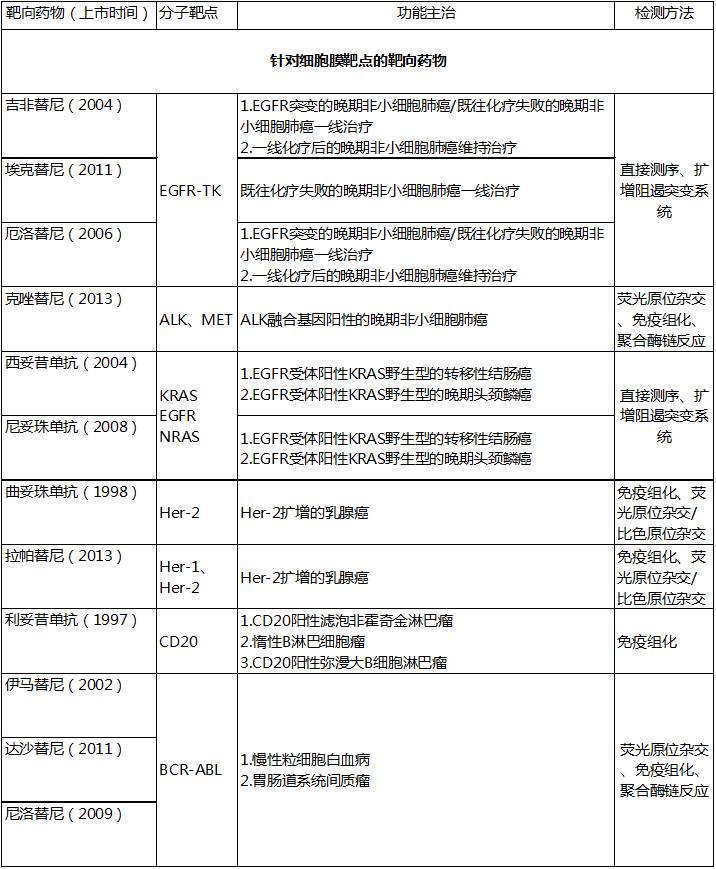
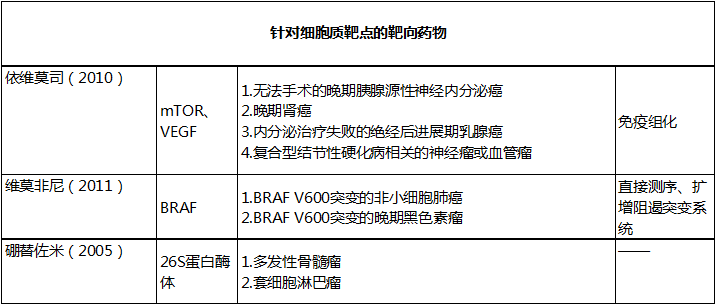
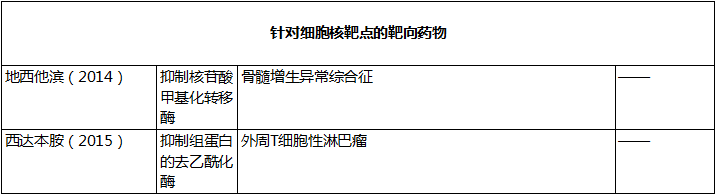
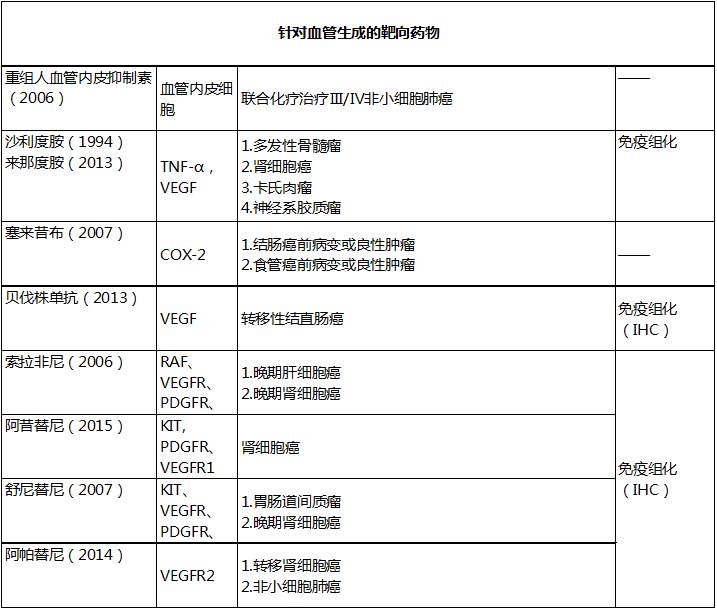
一表读懂:靶向药物全新总结
2016-09-03 王少军 肿瘤时间
靶向药物是指干扰肿瘤各个过程的特定分子而实现抑制或阻断肿瘤进展的药物,其发挥功能的基础是正常细胞和肿瘤细胞的差异之处,这使得靶向药物的特异性强而副作用小。靶向药物是精准治疗的「先锋」其诠释了「标准化」治疗为基础的「个体化」治疗原则。而「个体化」治疗的前提条件是因为个体差异而进行的分子靶点检测。个体分子靶点检测包括:(1)个体基因突变靶点的检测,(2)个体基因扩增靶点的检测,(3)个体基因融合靶点的
靶向药物是指干扰肿瘤各个过程的特定分子而实现抑制或阻断肿瘤进展的药物,其发挥功能的基础是正常细胞和肿瘤细胞的差异之处,这使得靶向药物的特异性强而副作用小。靶向药物是精准治疗的「先锋」其诠释了「标准化」治疗为基础的「个体化」治疗原则。
而「个体化」治疗的前提条件是因为个体差异而进行的分子靶点检测。个体分子靶点检测包括:(1)个体基因突变靶点的检测,(2)个体基因扩增靶点的检测,(3)个体基因融合靶点的检测。
靶向药物飞速发展但是目前传统化疗仍处不可替代的位置。靶向药物主要分为两类:大分子单克隆抗体和小分子激酶抑制剂。激酶靶点包括(1)酪氨酸激酶,(2)丝氨酸/苏氨酸激酶,(3)其他蛋白酶。
目前激酶靶点主要是针对酪氨酸激酶。酪氨酸激酶抑制剂分为:受体类酪氨酸激酶抑制剂(主要针对 EGFR、VEGF、PDGF、FGFR 家族)和非受体酪氨酸激酶抑制剂(主要针对 ABL、JAK、SRC、FAK 家族)。
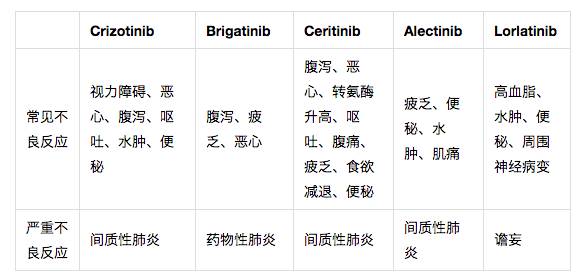
随着分子细胞水平研究的深入相信会有越来越多的靶向药物造福患者。下表首次按细胞结构列出目前中国上市的临床获益的靶向药物。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












总结的很好,学习了
77
学习了,好
68
很好的总结
62
学习了,了解了!
66
学习了,了解了!
66
靶向药物造福患者!
25
学习起来
20
实用,收藏了
19