Lancet neurology:脑淀粉样血管病的波士顿标准2.0版新标准研究
2022-08-02 网络 网络
波士顿标准V2.0纳入了新出现的CAA的MRI标志物,在50岁及以上出现自发性脑内出血、认知障碍或短暂的局灶性神经发作的患者队列中,提高了敏感性而不影响其特殊性。
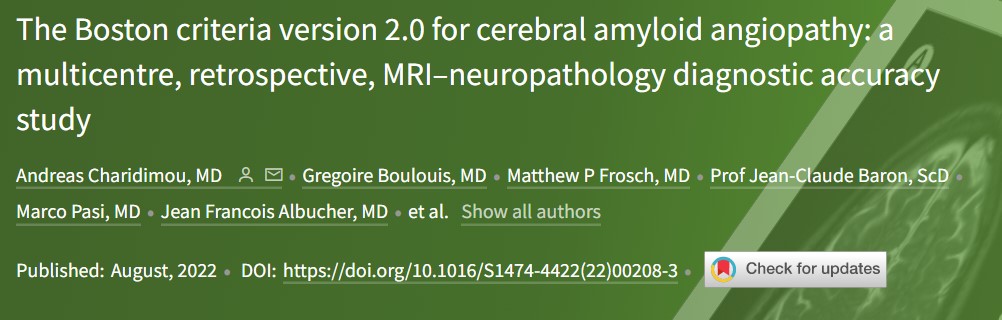
大脑淀粉样血管病(CAA)是一种与年龄有关的小血管疾病,其病理特征是淀粉样β蛋白在脑血管壁上的逐渐沉积。波士顿标准在全球范围内被用于CAA的体内诊断,但自2010年以来,在其他MRI标志物出现之前,该标准一直没有被更新。为此,近期发表在Lancet neurology杂志上的研究报告了一项国际合作研究,旨在更新并从外部验证波士顿诊断标准在CAA临床表现的全部范围。
在这项基于医院的多中心、回顾性、MRI和神经病理学诊断准确性研究中,研究人员对参加国际CAA协会的机构所掌握的临床、放射学和组织病理学数据进行了回顾性分析,以制定更新的波士顿标准并确定其在不同人群和临床表现中的诊断准确性。10个北美和欧洲的学术医疗中心确定了50岁及以上具有潜在CAA相关临床表现(即自发性脑内出血、认知障碍或短暂的局灶性神经发作)的患者,可用脑部MRI和组织病理学评估来诊断CAA。
在马萨诸塞州综合医院就诊的401名可能符合条件的患者中,有218人符合纳入分析的条件;在来自其他中心的160名患者数据中,有123人被纳入。利用推导出的队列,研究得出了可能的CAA的临时标准,要求至少存在两个严格意义上的脑叶出血性病变(即脑内出血、脑微出血或皮质浅层蛛网膜病灶)或至少一个严格意义上的脑叶出血性病变和至少一个白质特征(即半卵圆中心严重可见的血管周围间隙或多点模式的白质高信号)。这些标准的敏感性和特异性在派生队列中为74.8%和84.6%,在时间验证队列中为92.5%和89.5%。在地理验证队列中为80.2%和81.5%,在所有以尸检为诊断标准的患者中为74.5%和95.0%。在所有以尸检为诊断标准的人中,可能的CAA的波士顿标准v2.0版具有更高的准确性(敏感性64.5%.;特异性95.0%.;AUC 0.798)。

波士顿标准V2.0纳入了新出现的CAA的MRI标志物,在50岁及以上出现自发性脑内出血、认知障碍或短暂的局灶性神经发作的患者队列中,提高了敏感性而不影响其特殊性。未来的研究将需要确定v.2.0标准在所有患者和临床表现中的普遍性。
参考文献:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言















#新标准#
52
#血管病#
71
#脑淀粉样#
47
#Lancet#
36
#Neurol#
44
#脑淀粉样血管病#
48
lancet上果然牛,感谢梅斯更新及时
26