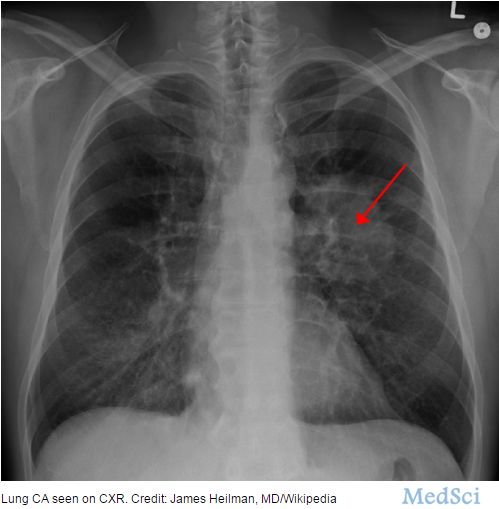
晚期非小细胞肺癌各种治疗方案汇总及常见问题
2017-03-24 佚名 海得康海外就医
2017.2版中,免疫药物——PD1抑制剂Keytruda被FDA批准,用于一线治疗(新诊断的癌症患者,首先接受的治疗)!Keytruda一线并不适用于所有肺癌,目前只针对“PD-L1高表达”,“无EGFR或ALK突变”的“非小细胞肺癌”。随着免疫疗法加入,非小细胞肺癌一线治疗用药将越来越精确:a.有EGFR,ALK等主流突变,考虑优先使用靶向药物(EGFR-易瑞沙、特罗凯、AZD9291等,AL
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#非小细胞#
24
#治疗方案#
20
#常见问题#
33
这个值得收藏,
70
学习了,分享了
68