Neurology:多发性硬化症患者结直肠癌生存率
2021-09-17 MedSci原创 MedSci原创
在结直肠癌诊断后的早期,MS患者的总体和癌症特异性生存率较低。需要进一步研究以确定哪些因素可能导致这些糟糕的结局。
近日,神经病学领域权威取杂志Neurology上发表了一篇研究文章,研究人员旨在使用回顾性匹配队列设计检验以下假设:即多发性硬化症(MS)患者在确诊结直肠癌后的总体和癌症特异性生存率低于无MS患者。

研究人员使用曼尼托巴省和安大略省基于人群的行政数据,并通过验证的病例定义确定了MS患者,同时将这些队列与癌症登记处进行联系,以确定结肠直肠癌患者。研究人员根据结直肠癌患者的出生年份、性别、癌症诊断年份和地区以4:1匹配了非MS患者,并使用Cox比例风险回归来比较调整癌症诊断年龄、癌症诊断年份、收入、地区和Elixhauser合并症评分的队列之间的全因生存率。
 研究人员使用特定原因的风险模型比较了队列之间的癌症特异性生存率。研究人员使用随机效应荟萃分析汇总了各省的结果,并使用来自安大略省的子队列进行补充分析,根据癌症分期和残疾状态进行了调整,同时根据家庭护理或长期医疗服务的使用情况进行了衡量。
研究人员使用特定原因的风险模型比较了队列之间的癌症特异性生存率。研究人员使用随机效应荟萃分析汇总了各省的结果,并使用来自安大略省的子队列进行补充分析,根据癌症分期和残疾状态进行了调整,同时根据家庭护理或长期医疗服务的使用情况进行了衡量。
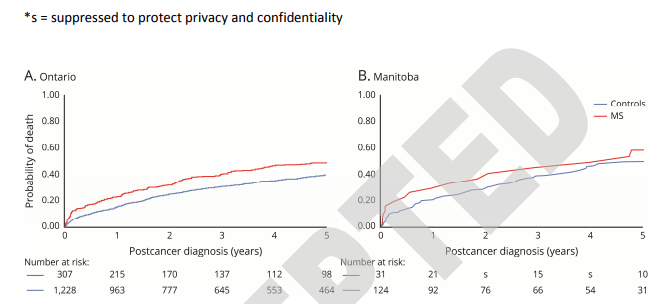
研究人员纳入了338例MS病例和1352例结直肠癌对照者。癌症诊断时的平均(SD)年龄为64.7(11.1)岁。调整后,MS与全因死亡风险增加相关,在诊断后六个月风险最高(风险比[HR]为1.45;95%CI为1.19-1.76),然后随着时间的推移下降(1年HR为[95%CI]:1.34[1.09-1.63],2年:1.24[0.99-1.56];5年:1.10[0.80-1.50])。仅在诊断后6个月,MS与癌症特异性死亡增加相关(HR为1.29;95%CI为1.04-1.61)。调整癌症分期后,MS与全因死亡(1.60;95%CI为1.16-2.21)和癌症特异性死亡(HR为1.47;95%CI:1.02,2.12)风险增加。在调整残疾状态后,MS与全因死亡(HR为1.37;95%CI为0.97-1.92)和癌症特异性死亡(HR为1.34;95%CI为0.91-1.97)之间的关联部分有所减弱.
在结直肠癌诊断后的早期,MS患者的总体和癌症特异性生存率较低。需要进一步研究以确定哪些因素可能导致这些糟糕的结局。
原始出处:
Susanna C. Larsson.et al.Colorectal Cancer Survival in Multiple Sclerosis: A Matched Cohort Study.Neurology.2021.https://doi.org/10.1212/WNL.0000000000012634
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#多发性#
40
#Neurol#
43
#硬化症#
38
很不错的学习软件
69
#生存率#
32
#结直肠#
40
真的要认真学习了
67
学习学习
61
厉害
65
学习
69