Gynecol Oncol:治疗前中性粒细胞与淋巴细胞的比率与子宫内膜癌患者的 OS 相关
2022-08-25 MedSci原创 MedSci原创
最近一项研究的结果表明,治疗前中性粒细胞与淋巴细胞的比率低于 6 与改善子宫内膜癌患者的总体生存率相关。
最近一项研究的结果表明,治疗前中性粒细胞与淋巴细胞的比率低于 6 与改善子宫内膜癌患者的总体生存率相关。
根据发表在妇科肿瘤学上的一项研究,在接受免疫治疗的复发性子宫内膜癌患者中观察到改善的总生存期 (OS),这些患者在基线时中性粒细胞与淋巴细胞的比率 (NLR) 低于 6。
NLR 低于 6 的患者与比率为 6 或更高的患者相比 OS 有所改善(P <.05),与 41 相比,1 年生存概率为 69%(95% CI,58%-82%) %(95% CI,26%-67%)。
该分析共检查了来自单一机构的 106 名患者,其中 77 名(72.6%)的 NLR 小于 6。58.5% 的患者发现子宫内膜样病变,74.5% 的患者有 3 个或更多的转移部位,36.8 % 在免疫治疗之前接受过 2 种或更多的治疗。在 49.1% 的患者中观察到错配修复 (MMR) 缺陷,两组之间的错配修复状态相似。
在 MMR 缺陷型肿瘤患者中,94.3% 的患者接受了派姆单抗单药治疗(Keytruda),78.7% 的 MMR 正常型肿瘤患者接受了乐伐替尼(Lenvima)联合派姆单抗治疗。
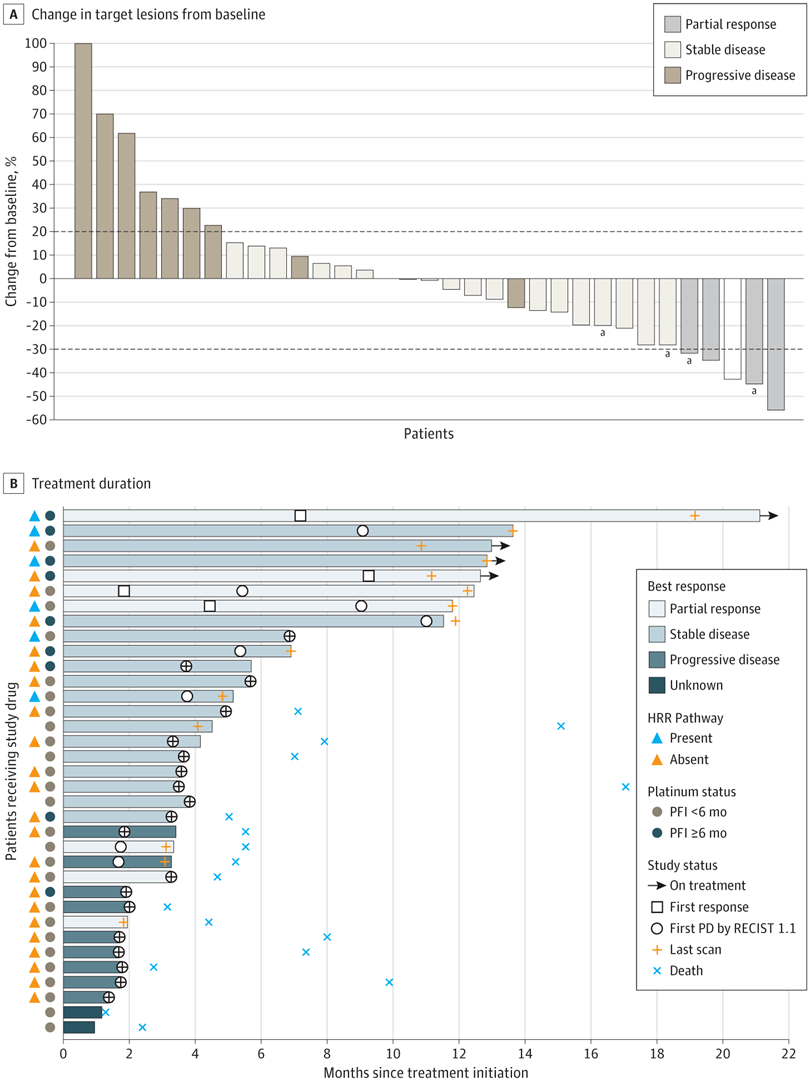
总体而言,40.2% 的 NLR 小于 6 的患者在第一次放射影像学评估时对治疗有反应,其中 29.9% 的患者有部分反应 (PR),10.4% 的患者有完全反应 (CR)。在 NLR ≥ 6 的患者中,31% 的患者有反应,其中 27.5% 有 PR,3.4% 有 CR (P = .69)。在 MMR 缺陷的患者中,50% 的 NLR 低于 6 的患者有反应,34.2% 的患者有 PR,15.8% 的患者有 CR,而 NLR ≥ 6 的患者中有 35.7% PR 率为 35.7%,无 CR (P = .52)。此外,NLR 低于 6 的 MMR 熟练亚组的总体反应率为 33.3%,其中 27.3% 有 PR,6.1% 有 CR,而 NLR ≥ 6 的患者为 28.5%,其中 21.4% PR 率和 7.1% CR 率 (P >.095)。
研究人员发现整个队列的无进展生存期没有差异(PFS;P = .93)。 NLR 小于 6 组的中位 PFS 为 9.3 个月,而 NLR ≥ 6 组为 7.4 个月。 NLR 小于 6 的患者接受中位数为 6 个周期的免疫治疗,而 NLR 为 6 或更多组的患者接受 5 个周期。
NLR 小于 6 的患者中位总生存期为 26 个月,而 NLR ≥ 6 组的中位总生存期为 11 个月(P = .003)。在按 MMR 状态分层的亚组中,PFS 没有观察到差异,但两组的 OS 都受到 NLR 的影响。对于 MMR 缺陷患者,NLR 小于 6 组的中位 OS 为 45.0 个月,而 NLR ≥ 6 组为 13.4 个月(P = .01)。对于 MMR 熟练且 NLR 小于 6 的患者,中位 OS 未达到,而 NLR ≥ 6 的患者为 7.3 个月(P = .01)。
在少于 6 组的 NLR 中,总共 19.5% 的患者经历了 3/4 级不良反应,而在 6 组或更多组的 NLR 中,这一比例为 17.2%。在两组患者中,大多数患者未接受进一步治疗,但 38.9% 的 NLR 小于 6 的患者接受了后续治疗,而 13.8% 的 NLR 为 6 或更高的患者接受了后续治疗 (P = .01)。患者大多接受了 1 种额外的激素治疗或细胞毒化疗,除 3 例外,情况都是如此。
原始出处:
Barrington DA, Calo C, Baek J, et al. Beyond mismatch repair deficiency? Pre-treatment neutrophil-to-lymphocyte ratio is associated with improved overall survival in patients with recurrent endometrial cancer treated with immunotherapy. Gynecol Oncol. Published online July 27, 2022. doi:10.1016/j.ygyno.2022.07.010
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#内膜#
45
#Oncol#
47
#NEC#
0
学习了
38
#中性粒细胞#
53
#淋巴细胞#
0