HR+HER2-晚期乳腺癌CDK4/6i失败后治疗模式新探索
2022-08-23 网络 网络
在2022年“天津国际乳腺癌大会”会议上,福建省肿瘤医院乳腺内科的刘健教授以《HR+HER2-晚期乳腺癌CDK4/6i失败后治疗模式新探索》为题,对相关内容进行了详细的讲解。
靶向CDK4/6抑制剂已成为HR+/HER2-晚期乳腺癌的标准治疗方案,但临床实践中常常存在CDK4/6i失败的患者,那么这些患者又该如何进一步治疗呢?
在2022年“天津国际乳腺癌大会”会议上,福建省肿瘤医院乳腺内科的刘健教授以《HR+HER2-晚期乳腺癌CDK4/6i失败后治疗模式新探索》为题,对相关内容进行了详细的讲解。
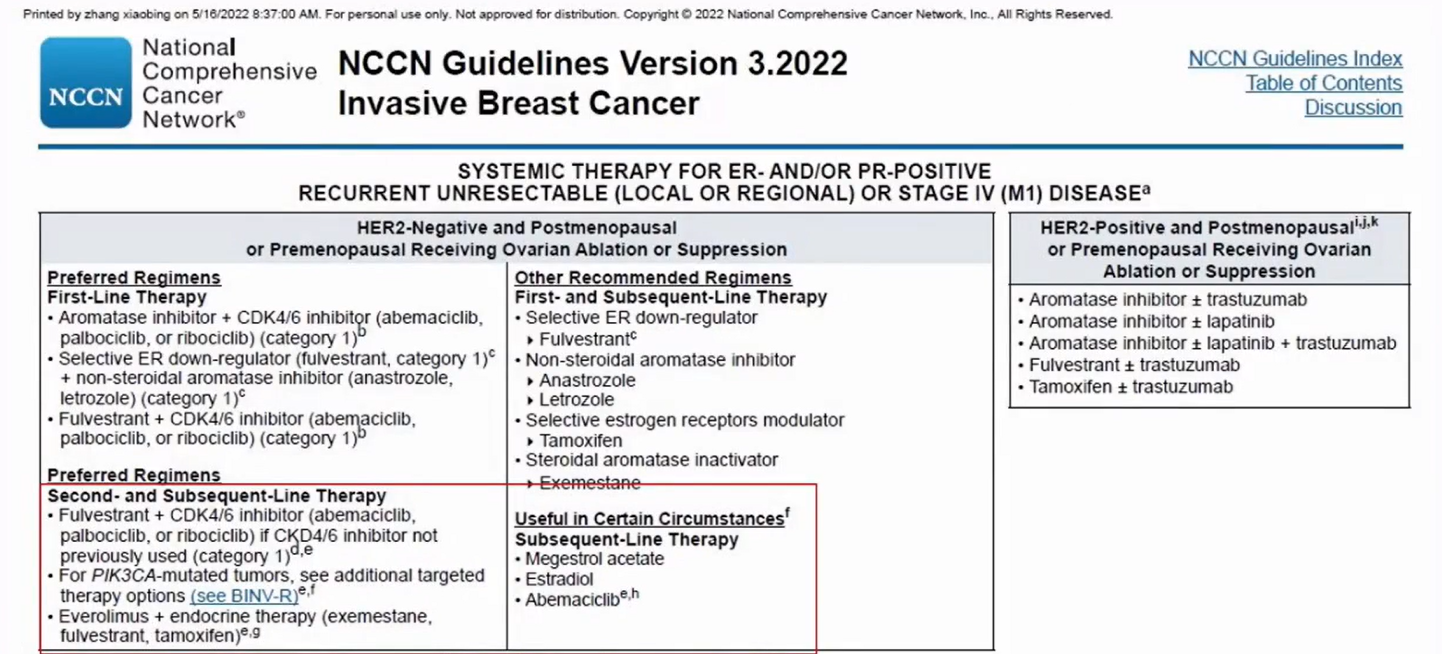
2022NCCN指南对HR+/HER2-乳腺癌患者的治疗进行了推荐
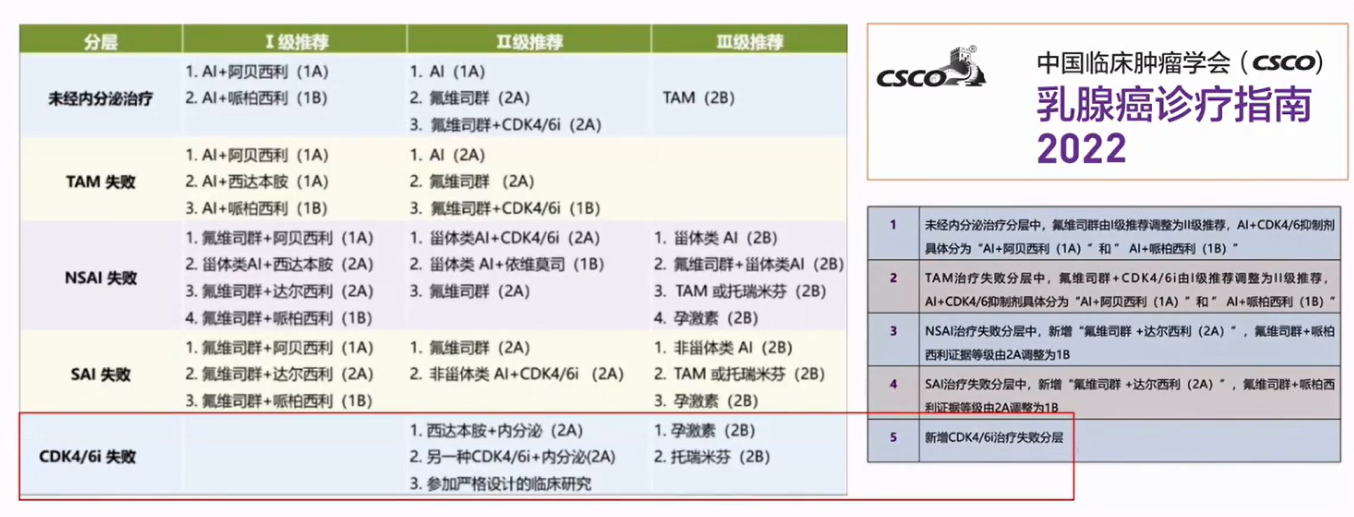
CSCO-BC指南对HR+/HER2-晚期乳腺癌分层制定了细则,其中新增了CDK4/6i失败的分层,对这类患者的治疗进行了指导。
那么对于HR+HER2-晚期乳腺癌CDK4/6i失败后有什么规范的治疗模式?
一、CDK4/6i失败后治疗模式之一:化疗
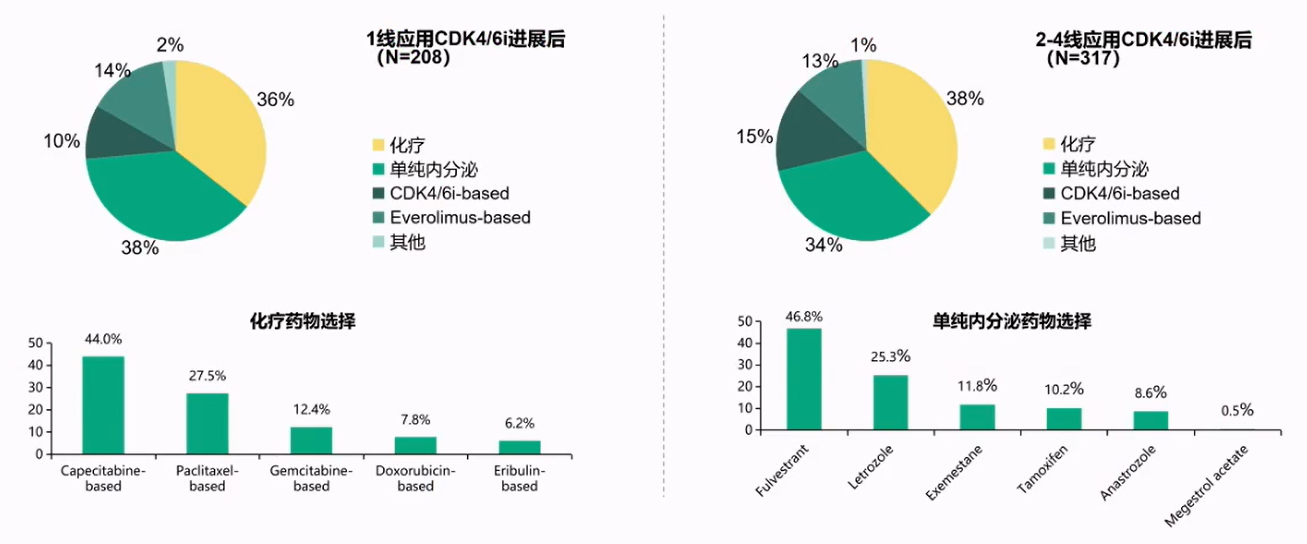
一项来自美国的真实世界研究,纳入MarketScan数据库中2012年-2017年间525名接受CDK4/6抑制剂后出现进展的绝经后HR+/HER2-mBC患者(1线患者208名,2-4线317名),分析其后续治疗选择。发现无论是一线进展,还是二线后进展,后续的治疗仍有三分之二以内分泌治疗为主。
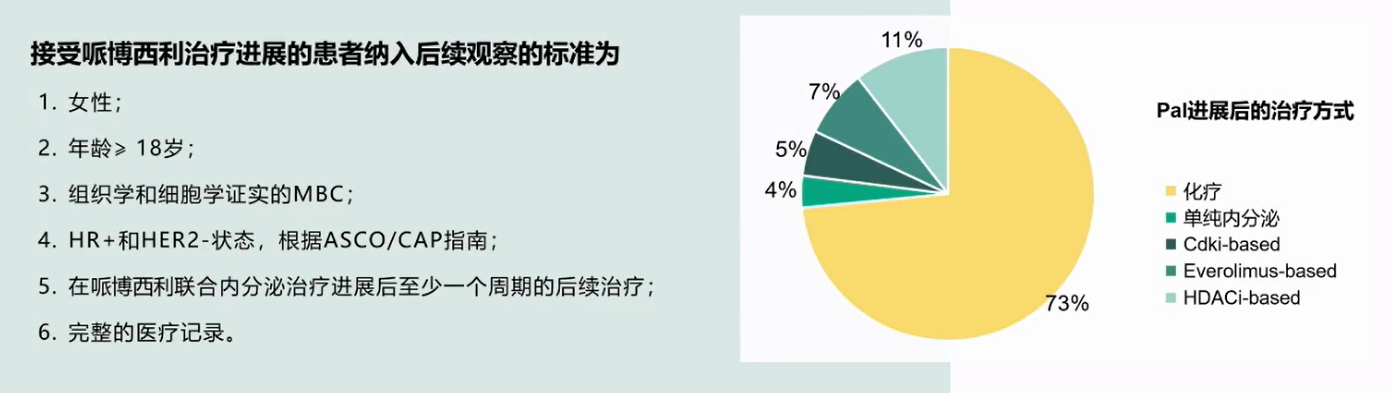
一项纳入了中国5家医院(复旦大学附属肿瘤医院、江苏省人民医院、浙江省肿瘤医院、湖南省肿瘤医院、上海交通大学附属瑞金医院)200名HR+/HER2-乳腺癌患者,观察其在2017年8月-2020年4月间接受过Palbociclib治疗进展后的治疗模式,疗效与安全性。结果发现中国人群的化疗比例很大,达到73%,但是在既往对哌柏西利治疗敏感的患者中观察到后续使用内分泌获益更大的趋势。
戈沙妥珠单抗(SG)是全球首个且唯一获批Trop-2ADC,独特的药物设计包括靶向Top-2,人源化lgG1抗体,稳定的连接子及高效能载药。
TROPiCS-02是一项针对SG治疗HR+/HER2-乳腺癌的3期研究,主要终点是盲态独立中心评估(BICR)评估意向治疗分析人群的PFS(RECIST v1.1),既往CDK4/6i治疗失败所占患者的比例达到98%,结果发现SG相较TPC(卡培他滨、艾立布林、长春瑞滨或吉西他滨)治疗PFS显著改善,疾病进展死亡的风险降低34%。
DESTINY-Breast04是一项针对HER2-low mBC的Ill期研究,对比T-DXd与TPC(卡培他滨、艾立布林、吉西他滨、紫杉醇、白蛋白结合型紫杉醇)单药化疗的治疗效果,既往CDK4/6i治疗失败所占患者的比例达到64%-71%。、HR+和所有患者中的PFS、OS在T-DXd组明显优于TPC组,实现PFS和OS双获益。HR+/HER2-乳腺癌患者中确认的客观缓解率(ORR)在T-DXd组都明显优于TPC组。
二、CDK4/6i失败后治疗模式之二:CDK4/6i跨线使用
在哌柏西利治疗进展后阿贝西利跨线治疗中,整体患者的mPFS达到5.3m。
瑞波西利:MAINTAIN试验在经抗雌激素治疗联合细胞周期蛋白依赖性激酶4/6抑制剂治疗后进展的不可切除或转移性激素受体阳性、HER2阴性乳腺癌患者中,使用氟维司群或依西美坦联合/不联合瑞波西利治疗的随机、Ⅲ期试验,瑞波西利+ET对比安慰剂+ET发现两组PFS差异有统计学意义(5.29个月vs2.76个月)。
2020ESMO国际共识指南的晚期乳腺癌(ABC5)第5版指南中74不建议跨线使用,指南明确指出只有对于之前没有用过CDK4/6i的患者,在一线治疗进展后才可以使用,否则需要更换其他的治疗方案。
NCCN乳腺癌指南(2022.V2)指出CDK4/6抑制剂治疗期间出现疾病进展,支持使用其他CDK4/6抑制剂继续治疗的数据有限。
中国抗癌协会乳腺癌诊治指南与规范(2021版)的激素受体阳性HER2阴性MBC的治疗原则指出CDK4/6抑制剂跨线使用的证据有限,需谨慎选择。
不同安全性的CDK4/6抑制剂在特殊情况下可以进行替换。

当发生严重中性粒细胞减少症时不同CDK4/6抑制剂间替换策略如下:

非血液学不良反应中,不同CDK4/6抑制剂间替换:

达尔西利归引入哌啶结构避免潜在的肝脏毒性:谷胱甘肽,是由谷氨酸、半胱氨酸和甘氨酸结合,是含有巯基的三肽。谷胱甘肽(尤其是肝细胞内的谷胱甘肽)能参与生物转化作用,从而把机体内有害的毒物转化为无害的物质,排泄出体外,具有抗氧化作用和整合解毒作用,能帮助保持正常的免疫系统功能。达尔西利引入哌啶结构,消除了谷胱甘肽捕获风险,避免潜在的肝脏毒性。
三、CDK4/6i失败后治疗模式之三:换不同作用机制的靶向药物
BOLERO-5是一项双盲、随机、Ⅱ期研究,在中国绝经后来曲唑或阿那曲唑治疗后进展的ER+HER2-局部晚期、复发性女性中,评价EVE+AI治疗的疗效。患者以1:1的比例随机接受EVE(10mgqd)+AI(25mgqd)或安慰剂(PBO)+AI(25mgqd)主要终点:无进展生存期PFS)。结果显示,无论是研究者评估还是BIRC评估,依维莫司联合AI相比AI单药治疗的患者中位PFS均延长。
TRINIT-1研究是一项多中心、开放、单臂、Ⅰ/Ⅱ期研究,纳入104例HR+HER2-晚期乳腺癌患者,其中96例既往接受过CDK4/6抑制剂治疗,患者在进展后接受CDK4/6抑制剂+mTOR抑制剂+A1三药联合治疗方案,探讨CDK4/6抑制剂治疗进展后接受三药方案的疗效。结果显示,在24周时患者的临床获益率可达到41%,超过预设主要终点(>10%),中位PFS5.7个月,数据截止时中位0S未达到(95%CI:NE,NE)。
Sapanisertib是mTOR激酶的口服强效高选择性三磷酸腺苷竞争性抑制剂,对mTORC1和nTORC2具有双重特异性。期、开放性、随机、三组研究探索与氟维司群单药治疗相比,在氟维司群联合每日一次(QD)或海周一次(QW)的sapanisertib,以评价联合治疗是否改善了结局,芳香化酶抑制剂治疗期间或治疗后进展的ER+/HER2-晚期或转移性乳腺癌绝经后女性患者。单药氟维司群组PFS为3.5个月,而氟维司群+sapanisertib QD组为7.2个月,氟维司群+sapanisertib QW组为5.6个月两个联合治疗组因不良事件导致的治疗中止发生率高于氟维司群单药治疗组(分别为32%和36%vs4%)。
ACE研究是针对西达本胺联合依西美坦治疗HR+HER2-ABC的随机、双盲、安慰剂对照3期研究,纳入365例HR+HER2-ABC患者,随机分配至西达本胺+EXE组(n=244)和安慰剂+EXE组(n=121),整体患者中针对转移性疾病先前接受过1L以上治疗患者占57.5%(其中ET为47.7%,化疗30.1%),32.8%患者对先前ET治疗不敏感。发现主要研究终点PFS(7.4m vs 3.8m(研究者评估),9.2m vs 3.8m(IRC评估))有显著差异。
西达本胺治疗晚期乳腺癌2000例真实世界研究显示,PFS达到6.4个月。
E0C103A3101是一项恩替诺特联合依西美坦治疗HR+/HER2-ABC的3期研究,在中国人群再次验证HDACi+Ai的疗效。
刘健团队研究西达本胺治疗晚期乳腺癌的数据显示,中位PFS(非内脏转移Vs内脏转移)为9月vs 6月,将西达本胺作为各线治疗的中位PFS比较:1线(9m)vs2线(6m)vs≥3线(6m)。
PI3K抑制剂Alpelisib+氟维司群显著延长PIK3CA突变患者PFS。
2020ASCO BYLieve是一项2期,开放标签,3队列,非对照研究,目标是在既往CDK抑制剂治疗人群,评估Alpelisib+内分泌疗法(氟维司群或来曲唑)治疗伴PK3CA突变的HR+,HER2-晚期乳腺癌患者的有效性和安全性。结果表明CDKi+A队列达到主要终点(95%C1下限>30%),6个月时未发生疾病进展的存活患者比例为50.4%。
四、总结
有关HR+HER2-CDK4/6i失败后治疗模式:
化疗最常用,其中ACD药物有可能成新贵
PI3K/AKT/mTOR通路的抑制剂是新选择
CDK4/6i跨线使用有待新证据
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#HER2-#
56
#CDK4#
65
#CDK#
40
#CDK4/6#
35
#治疗模式#
46