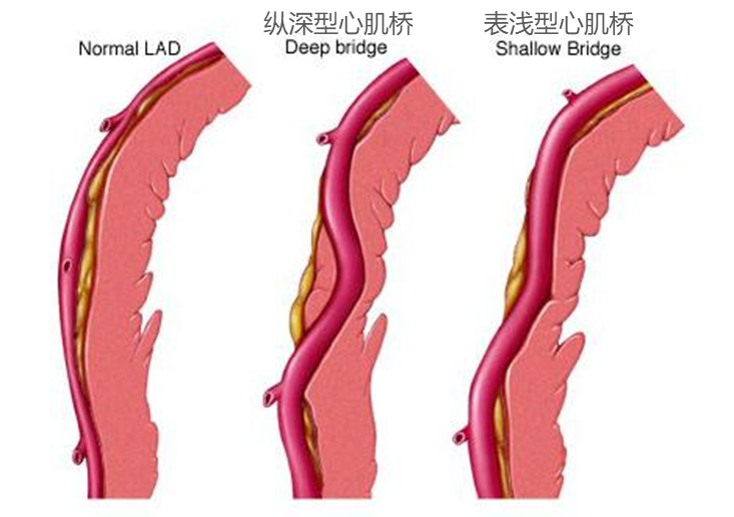
心肌桥(myocardial bridge,MB)是出生时即存在的冠状动脉先天性解剖异常,当一段心外膜冠状动脉走行于心肌内,这部分心肌形状似“桥”,被称为心肌桥,走行于心肌桥下的冠状动脉被称为壁冠状动脉。
01 冠脉造影
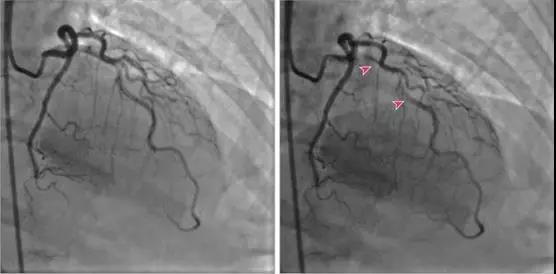
若发现冠脉收缩期狭窄或合并舒张期松弛延迟现象,则提示有心肌桥存在。但冠脉造影只能检出那些对冠脉血流产生显著影响的心肌桥。心肌桥的检出与其长度、肌桥纤维的走行方向、心肌桥与相关动脉间的组织有关。有些心肌桥由于其近端的冠脉几乎完全闭塞或动脉粥样硬化产生的固定性狭窄限制了冠脉的血流灌注而掩盖了其收缩期狭窄,或由于血管痉挛的存在,造影很难发现。冠脉造影常不能发现心肌桥处的动脉粥样硬化性狭窄。
心肌桥常见于左前降支(LAD)的中段,冠状动脉造影的检出率为1.5%~16%,尸体解剖的检出率为80%
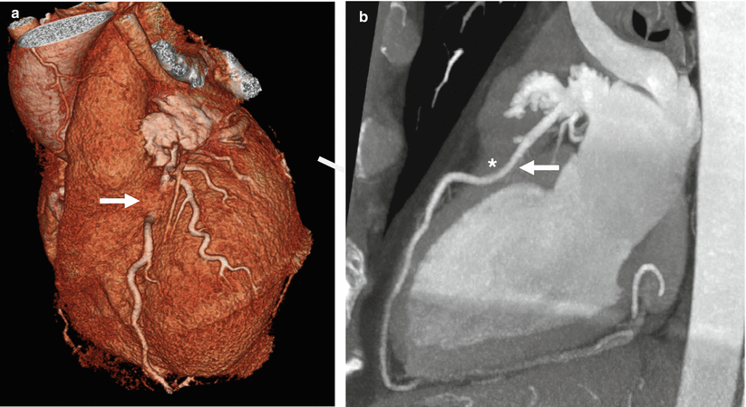
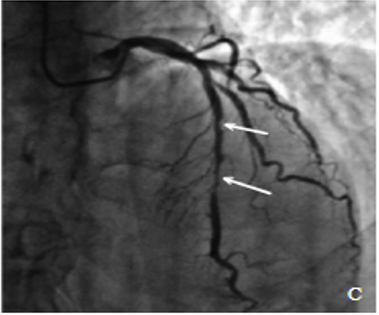
通常对于肌桥的诊断依赖于冠脉造影和冠状动脉CTA。在冠脉造影中,肌桥存在导致冠状动脉呈现线状、串珠状或蚯蚓状,称之为“挤牛奶征”。
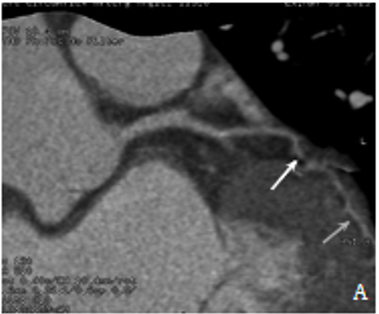
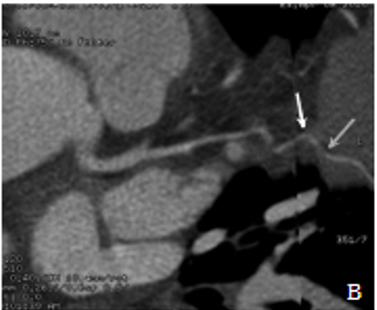
图A:左冠回旋支心肌桥的冠状动脉(舒张期)CTA表现
图B:左冠回旋支心肌桥的冠状动脉(收缩期)CTA表现
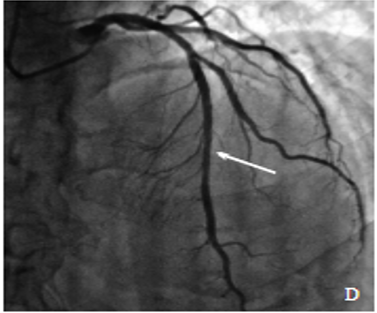
图C:冠状动脉造影术收缩期的桥血管狭窄程度
图D:舒张期的桥血管恢复正常(挤牛奶征)
02 冠脉内多普勒检查
发现心肌桥部分冠脉血流速度在舒张早期显著升高呈一峰值,很快又下降,继之呈一平台,直至收缩期再次下降。峰值的出现是由于冠脉内最大灌注压的存在,并相应出现血管面积的持续减小,导致心肌桥两端出现显著的压力阶差,当心肌桥舒张期松弛时,两端压力阶差消失,血管面积迅速扩大,血流速度也很快下降。
03 血管内超声
可发现心肌桥近端冠脉内常有动脉粥样硬化形成。冠脉内多普勒探得冠脉内血流储备减少。
心肌桥得不到相应的处理,可为近端血管粥样硬化的发生创造便利条件,并增加急性冠状动脉综合征的发生风险。
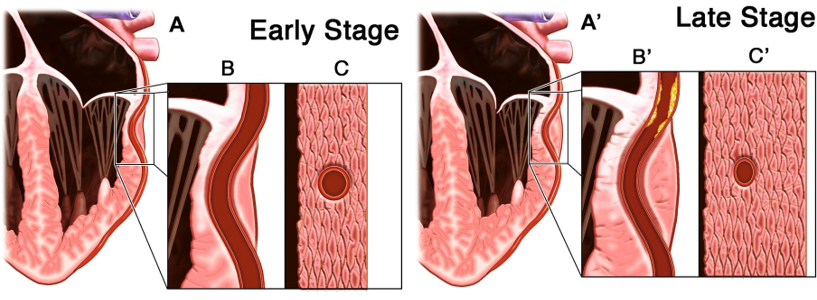
早期冠脉无粥样硬化,心肌桥影响不大,随着动脉粥样硬化的进展,心肌常伴有肥大,缺血症状会加重。
临床表现
心肌桥的临床表现与分型密切相关。
1.表浅型:因心肌桥薄而短,对冠脉血流影响较小,多数可无心肌缺血症状及相应的心电图改变。
2.纵深型:因心肌桥厚而长,对冠脉血流影响大,而出现心绞痛,心电图出现心肌缺血的ST-T改变。如果心肌桥并发冠脉粥样硬化继发血栓形成或斑块脱落,即可能出现心肌梗死的临床症状及相应的心电图改变。心肌桥合并快速型心律失常时更易出现心肌缺血。
大多数心肌桥不引起临床症状,出现的症状主要表现为:心绞痛、急性心肌梗死;房室传导阻滞;心力衰竭;猝死。
心肌桥在肥厚型心肌病患者中很常见,有心肌桥者比没有心肌桥者有更频繁的胸痛、心脏骤停、室性心律失常、运动时收缩压下降、运动时sT段明显压低和 QT间期离散度(QTc)增加发生率,且5年存活率明显降低。
大多数心肌桥患者心电图检查无明显异常,有临床症状患者可出现胸导联V3 ~V6或V4 ~V6缺血性ST-T段异常改变。部分心肌桥患者有早期复极综合征的表现。动态心电图有可能发现一过性心肌缺血表现,运动负荷心电图也可检出心肌桥患者的心肌缺血。
治疗
药物治疗
β受体阻滞剂和非二氢吡啶钙通道阻滞剂是症状型心肌桥一线治疗的首选药物。单纯的血管扩张剂不建议使用,硝酸酯类已被证明会引起继发性心动过速,加速其近端动脉粥样硬化的形成。
冠状动脉内支架置入术
持续性心绞痛患者在应用β受体阻滞剂治疗效果不显著时,可选用冠状动脉内支架置入术,但无法保证患者的远期疗效,且术后可能发生支架狭窄或闭塞的现象。
有研究结果显示,心肌桥患者行支架治疗7周后,发生支架内在狭窄的概率为46%。此外,支架置入术较药物治疗更易诱发严重心绞痛。
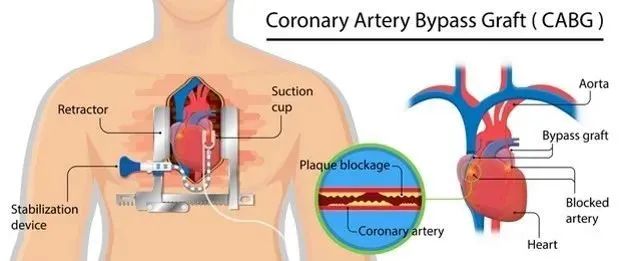
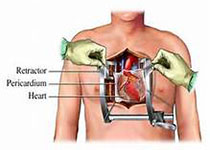
冠状动脉旁路移植术
当患者出现如下情况时,需要尽快接受冠状动脉旁路移植术治疗:
(1)经冠状动脉内支架置入术治疗后仍伴有顽固性心绞痛;
(2)冠状动脉近端狭窄且斑块不稳定;
(3)心肌桥紧密粘连于壁血管。
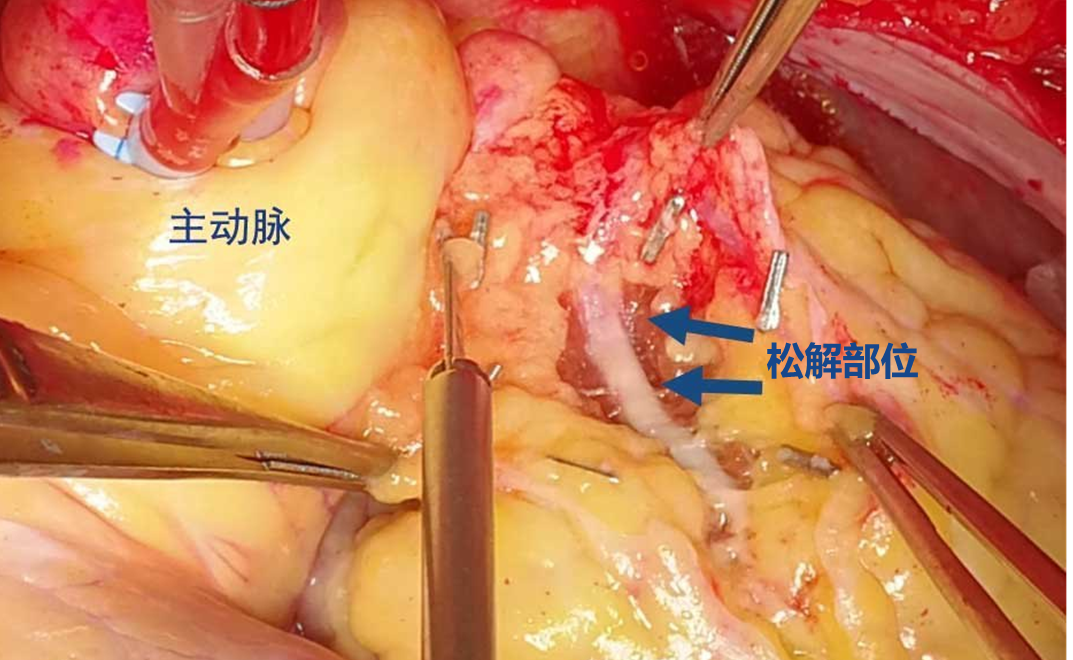
心肌桥切开松解术
适用于治疗冠状动脉浅肌桥患者,可基本上解除患者心肌受到的压迫,且大部分患者治疗后胸痛症状会随之消失。需注意的是,因无法预知心肌桥内患者冠状动脉的走向,必要情况下过度切开患者心室壁,可能会引发右室穿孔进而导致室壁瘤形成,且术后瘢痕组织可在一定程度上加重局部压迫。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#冠脉CT检查#
47
优秀
47
学习了
44
学习了
55
好文章,学习了。
0
#CT检查#
38
#冠脉CT#
37
很棒,从各个角度分析,更深刻理解
63
科技的进步
42