Radiology: LI-RADS分类告诉你原发肝癌是哪种类型!
2019-04-27 shaosai MedSci原创
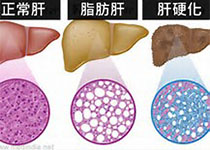
本研究旨在评价原发肝细胞肝癌患者LI-RADS对术后预后意义,验证LI-RADS 2017版在鉴别钆塞酸增强MRI检查中肝细胞肝癌(HCC)与肝内胆管细胞癌(IHCC)及混合肝细胞-胆管细胞癌(cHCC-CC)的价值。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#LI-RADS分类#
39
#RADS#
47
#ADS#
43
#LI-RADS#
46
肝癌,接下来就要细分了,对于体质好的病人,能否将PD-1类+抗血管新生+放疗等相结合,甚至有必要用TACE进行减负
50