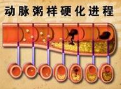
两岸三地学者共同在《Nature》发文,称发现动脉粥样硬化形成新机制
2016-12-15 佚名 天津医科大学官网
近日,天津医科大学、香港中文大学生物医学学院和台湾细胞及系统医学研究所合作完成的一项研究发现一种名为YAP/TAZ的血管内皮细胞转录调控因子与动脉粥样硬化形成及血管炎症有密切关系。 这一结果发表在《Nature》上。血管内皮细胞是形成血管内壁表面的细胞层,而YAP/TAZ是这种细胞的转录调控因子,YAP/TAZ本身被视为“癌基因”,会促进癌症的发生及发展。而本研究发现,抑制YAP/TAZ活性还有助
近日,天津医科大学、香港中文大学生物医学学院和台湾细胞及系统医学研究所合作完成的一项研究发现一种名为YAP/TAZ的血管内皮细胞转录调控因子与动脉粥样硬化形成及血管炎症有密切关系。 这一结果发表在《Nature》上。
血管内皮细胞是形成血管内壁表面的细胞层,而YAP/TAZ是这种细胞的转录调控因子,YAP/TAZ本身被视为“癌基因”,会促进癌症的发生及发展。
而本研究发现,抑制YAP/TAZ活性还有助推迟动脉粥样硬化形成及抑制血管炎症。且YAP/TAZ的活性受不同血流动力模式所调控。
研究者指出,血液在血管内的流动方式分为层流和湍流。层流带来的血液与血管内壁摩擦力(又称“剪切应力”)会抑制YAP/TAZ的活性,进而减弱促使炎症发生的JNK信号传导和相关炎症基因的表达,减少单核细胞对内皮细胞的黏附。反之湍流则会增加YAP/TAZ的活性, 从而造成炎症的发生。
此项研究还发现几种现有的降血脂或抗动脉粥样硬化药物可抑制YAP/TAZ转录激活,以他汀类效果最为显著。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#Nat#
32
#粥样硬化#
30
感染、炎症、增生
72
加强学术交流。
69
谢谢作者的分享
64
关注,值得借鉴
65