Hepatol Int:部分脾栓塞联合内镜治疗可明显降低脾亢的肝硬化患者的静脉曲张再出血率
2021-03-02 MedSci原创 MedSci原创
我国慢性乙肝病毒携带者人数达到了1.2亿,慢性乙肝患者3000万人
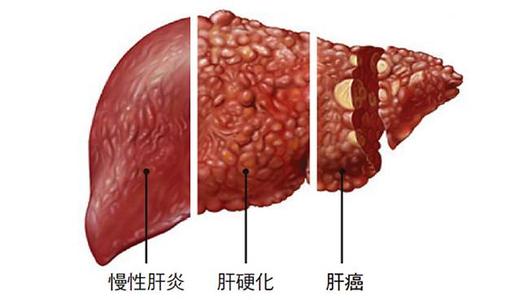
据世界卫生组织《2017年全球肝炎报告》:我国慢性乙肝病毒携带者人数达到了1.2亿,慢性乙肝患者3000万人。慢性乙肝控制不佳时往往会进展成肝硬化,甚至肝癌。肝硬化患者多会出现胃食管静脉曲张,静脉曲张是肝硬化患者消化道出血的主要原因。
目前,内镜联合部分脾栓塞术(PSE)治疗静脉曲张出血(VH)的全球研究有限。本研究目的是评价内镜联合PSE(EP)治疗对比内镜(E)治疗用作脾功能亢进的肝硬化患者二级预防VH的有效性和安全性。
这是一项多中心随机对照试验,招募了肝硬化伴脾功能亢进患者(血小板计数<10万/μL)和VH发作后恢复的患者,将受试患者随机1:1分为EP组和E组。主要终点是静脉曲张再出血,次要终点是严重的静脉曲张复发和死亡。检测各时间点的血液学指标、血清生化指标和Child-Pugh评分。
2016年6月-2019年12月,共纳入108例患者,其中102例接受了研究治疗方案(EP组和E组各51例)。
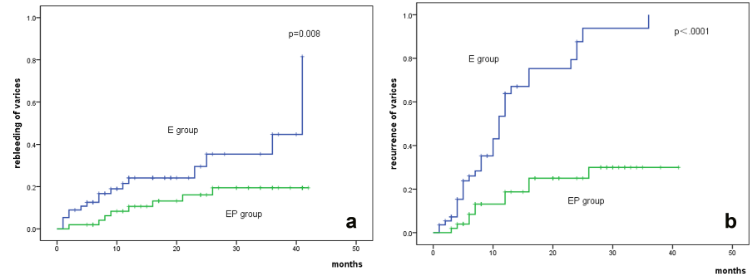
a.静脉曲张再出血率;b.静脉曲张复发率
随访2年,EP组静脉曲张再出血率明显低于E组(16% vs 31%,p<0.001)。EP组静脉曲张复发率也明显低于E组(22% vs 67%,p<0.001)。COX比例风险模型显示,分组是静脉曲张再出血(H=0.122,95%CI 0.055~0.270,p<0.001)和静脉曲张复发(危险性比,H=0.160,95%CI 0.077~0.332,p<0.001)的独立预测因子。
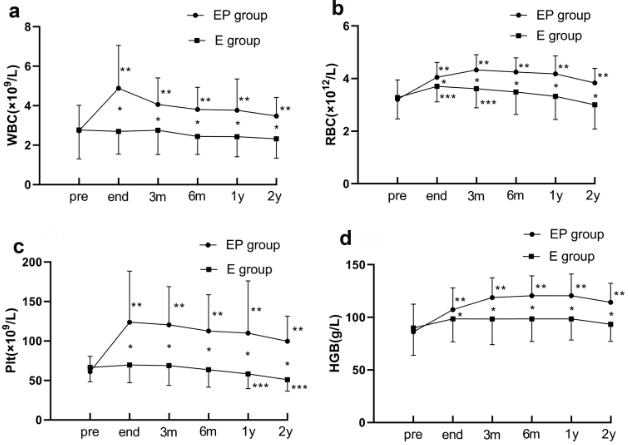
随访过程两组的WBC、RBC、血小板和HGB水平
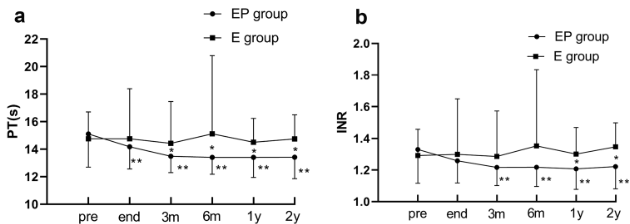
EP组的外周血细胞计数、Child-Pugh分级/评分、白蛋白浓度和凝血功能较E组在任何时间点均有显著改善(p<0.005)。
随访过程两组的凝血功能参数
综上,作为脾功能亢进的肝硬化患者静脉曲张的二级预防策略,内镜联合部分脾栓塞术治疗对预防静脉曲张再出血和静脉曲张复发的效果明显优于常规内镜治疗。此外,EP治疗还能显著提高患者外周血细胞计数和白蛋白浓度,改善凝血功能和Child-Pugh评分。
原始出处:
Sun Xin,Zhang Anzhong,Zhou Tao et al. Partial splenic embolization combined with endoscopic therapies and NSBB decreases the variceal rebleeding rate in cirrhosis patients with hypersplenism: a multicenter randomized controlled trial.[J] .Hepatol Int, 2021, 10.1007/s12072-021-10155-0
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#静脉#
36
学习了,谢谢分享
0
肝硬化患者出血率高
79
#内镜#
45
#EPA#
34
#内镜治疗#
53
好文章!
0
谢谢!最新的信息读起来就是收获大
60
提高技术质量,提高患者质量。
0
学习一下,我要积分
72