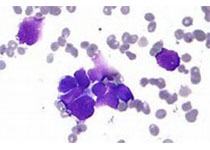
Blood:PD-1封闭可提高复发性/难治性经典霍奇金淋巴瘤患者的缓解率,并延长其缓解时间,但会增加其免疫毒性风险
2018-05-03 MedSci MedSci原创
对于不适合进行自体造血干细胞移植(HCT)或移植后复发的复发性/难治性(R/R)典型霍奇金淋巴瘤(cHL)患者,PD-1封闭是一种有效疗法。尽管抗PD-1单克隆抗体(mAbs)可提高缓解率、延迟缓解持续时间,但就目前的数据表明采用该疗法的大部分患者的病程终还是会进展。很多患者经抗PD-1 mAbs治疗后,即可接受异体HCT(allo-HCT),因此,在这种情况下,allo-HCT仍是目前唯一证实的
对于不适合进行自体造血干细胞移植(HCT)或移植后复发的复发性/难治性(R/R)典型霍奇金淋巴瘤(cHL)患者,PD-1封闭是一种有效疗法。尽管抗PD-1单克隆抗体(mAbs)可提高缓解率、延迟缓解持续时间,但就目前的数据表明采用该疗法的大部分患者的病程终还是会进展。很多患者经抗PD-1 mAbs治疗后,即可接受异体HCT(allo-HCT),因此,在这种情况下,allo-HCT仍是目前唯一证实的可治愈cHL的疗法。
但是,有报告提示在这种状况下,allo-HCT可能会增加早期移植相关毒性风险,可能是由于PD-1阻滞的持续效应导致的。而且,很多进行allo-HCT的R/R cHL患者在移植后会复发,而且多数情况下治疗选择有限。在近期研究中,再次证实PD-1阻滞可提高缓解率,但同时伴随免疫毒性风险增加。
对于PD-1封闭究竟是在allo-HCT前还是allo-HCT后应用仍存在很多问题,特别是涉及到PD-1封闭后allo-HCT的可行性、预后、最佳时间和方法时。
尽管前瞻性数据不足,但这些问题不可避免,而且必须由对晚期cHL患者进行日常护理的临床医生来解决。Charles Herbaux等人在此提供了一个工作组基于现有数据和经验的统一建议,以指导制定医疗决策,直到获得更为明确的数据。
原始出处:
Charles Herbaux,et al.Recommendations for managing PD-1 blockade in the context of allogeneic HCT in Hodgkin lymphoma: taming a necessary evil.Blood 2018 :blood-2018-02-811174; doi: https://doi.org/10.1182/blood-2018-02-811174
本文系梅斯医学(MedSci)原创编译,转载需授权!
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#复发性#
31
学习
50
#难治性#
29