Spine:腰骶关节四钉棒固定系统生物力学稳定性良好
2013-05-29 Spine dxy
脊柱后凸畸形,L5-S1 脊柱滑移,神经肌肉型脊柱侧凸畸形,老年性骨质疏松性脊柱侧凸畸形等均需要进行腰椎后路长节段联合骶骨固定,但即使目前内固定器械和技术均已达到了一个相对完善的程度,腰椎联合骶骨长节段固定的融合率仍是一个巨大的挑战,因腰椎和骶骨局部解剖特征,腰骶部独特的力学传递方式,骶骨骨质较差等原因,腰椎部不融合导致的钉棒松动断裂,假关节形成,矢状位不稳定等情况时有发生。 目前主流的两种腰骶
脊柱后凸畸形,L5-S1 脊柱滑移,神经肌肉型脊柱侧凸畸形,老年性骨质疏松性脊柱侧凸畸形等均需要进行腰椎后路长节段联合骶骨固定,但即使目前内固定器械和技术均已达到了一个相对完善的程度,腰椎联合骶骨长节段固定的融合率仍是一个巨大的挑战,因腰椎和骶骨局部解剖特征,腰骶部独特的力学传递方式,骶骨骨质较差等原因,腰椎部不融合导致的钉棒松动断裂,假关节形成,矢状位不稳定等情况时有发生。
目前主流的两种腰骶关节固定方式包括:腰椎+单一骶骨固定,腰椎+骶髂联合固定,尽管上述方法能取得不错的固定效果,但仍存在如前所述的较多问题;因此有学者近期报道采用四根钉棒系统进行腰椎和骶骨节段的固定,但目前研究报道较少,而关于其生物力学的特征目前尚无报道,近日来自中国中山大学医学院附属一院的学者就骶骨螺钉单独固定,骶骨螺钉联合髂骨螺钉固定,四钉棒固定系统三种方法固定腰骶椎关节后脊柱的生物力学稳定性进行了相关尸体学的研究,相关结论发表在spine杂志上。
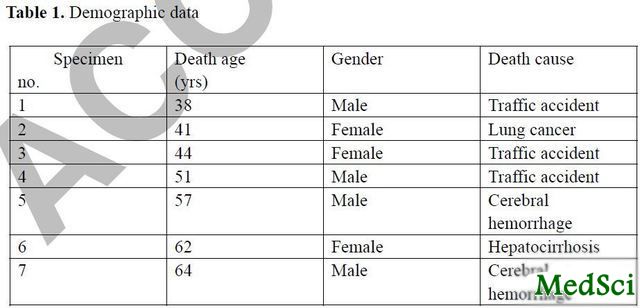
研究共收集7具尸体,4男3女,平均年龄51.3岁(如表1所示),所有尸体标本生前无明显的骨骼肌肉方面疾病,将尸体标本进行软组织剥离,只保留L1-L5及骨盆和其附属的软组织结构。试验前测量尸体标本的骨密度,确保各个尸体标本的骨质量无显著差异。
表1:尸体标本的统计学数据
将上述尸体标本分为四个组别:对照组,1例标本,不做任何处理;组别1,骶骨螺钉固定组,2例标本,常规固定方法;组别2,骶骨螺钉联合髂骨螺钉,2例标本,常规固定方法;组别3,四钉棒固定系统,固定方法:两侧各置入1枚S1螺钉及1枚骶翼(ala screw)螺钉,S1螺钉进针点在S1上关节突最下方外侧5mm,方向平行于S1 终板,并朝向前内侧10-15度;骶翼螺钉进针点在 S1螺钉更内侧点,朝前外侧30度,平行于骶翼,但不超过骶髂关节面,外侧长钉棒固定于S1螺钉和L2-L4椎体,内侧短钉棒固定于骶翼螺钉和L5椎体(如图1所示)。
将上述标本放置在测量装置中,四枚螺钉固定L1 头端,科式针固定骨盆处骶骨外的其他骨,成为一个头尾端固定,中间可活动得测量装置。通过该装置测量不同固定方法和完整标本的屈伸,侧弯及轴向旋转的运动度,并进行组间比较(如图2所示),在进行数据记录前先将所有标本进行3次load-unload循环预处理,以减少粘弹性对试验结果的影响。
测量数据包括:对照组及试验组的脊柱运动度(ROM)及中立位置(neutral zone),并按一下公式计算ROM及中立位置系数:neutral zone index = (neutral zoneintact- neutral zoneinstrumented) / neutral zoneintact; ROM index= (ROMintact - ROMinstrumented) /ROMintact。
试验结果如图3,4所示:在置入内固定装置前和后,患者的ROM有显著变化;所有试验组的ROM和对照组比较均出现ROM的减小;在侧弯运动中,组别2,3的ROM显著小于组别1,但组别2,3之间比较无显著差异;在屈伸运动中,组别1,3的ROM显著小于组别2,但组别1,3之间比较无显著差异;在轴向旋转运动中,组别3的ROM显著小于组别1,2,但组别1,2之间比较无显著差异。即组别3(四钉棒固定组)在所有方向上的运动幅度为所有组别中最小,固定最牢靠。
研究者认为,相较传统内固定的方法而言,四钉棒系统在对腰骶关节进行内固定时可以获得较好的力学稳定性。
编者按:脊柱节段内固定后的融合率一直是脊柱外科的难题,即使在腰椎、颈椎等节段中目前也没有任何技术能达到节段间100%的融合率。而在跨脊柱腰骶节段的固定中尤其如此,脊柱间不融合带来的临床后果较为严重,如何在现有的技术基础上提高脊柱融合率是外科学界努力的方向,节段间植骨融合,加用促进骨生长的辅助调节因子如BMP,更加符合脊柱生物力学的内固定方法等均有报道,但效果如何尚无定论。本研究对内固定的方法进行改进,并通过小样本尸体试验证实其内固定的稳定性较传统方法更好,但在临床实际应用中是否真的可以提高融合率需要后期更多的临床数据支持,我们拭目以待!
附
脊柱运动度定义:中立位置至最大负荷位置出现的角度变化
中立位置定义:预处理结束后脊柱的中立位置

Biomechanical Effect of Four-Rod Technique on Lumbosacral Fixation: An In Vitro Human Cadaveric Investigation.
Study Design
An in vitro biomechanical study of three lumbosacral fixation techniques in human cadaveric lumbar-pelvic spine models.
Objective
To compare the in vitro biomechanical effect of a novel four-rod lumbosacral reconstruction technique with conventional techniques in a human cadaveric lumbo-pelvic model, and to evaluate the benefit of adding supplementary rod fixation.
Summary of Background Data
Spino-pelvic fixation involving the sacrum remains a difficult clinical challenge. Numerous lumbo-pelvic reconstruction methods based on the Galveston two-rod technique have been proposed. Recently, a novel technique using supporting longitudinal rods across the lumbo-pelvic junction was reported. However, no comparative in vitro biomechanical testing was performed to evaluate the benefit of adding supplementary fixation at the L5-S1 levels.
Methods
Seven fresh-frozen cadaveric lumbar-pelvic spines were prepared and tested for bone mineral density (BMD). The intact cadavers underwent a flexibility test, followed by insertion of the instrumented construct. Three constructs were tested: S1 screws alone (group 1), S1 screws plus iliac screws (group 2), and the four-rod technique (group 3). Rotational angles of the L1-S1 and L5-S1 segments were measured to study the stability of the three lumbosacral fixation constructs compared with the intact spine. Nondestructive, multi-directional flexibility tests that included four loading methods followed by a destructive flexural load to failure were performed using an MTS machine. The lumbosacral peak range of motion (millimeters or degrees) and ultimate failure load (Nm) of the three reconstruction techniques were statistically compared using a one-way analysis of variance combined with a Studen Newman Keuls post hoc test.
Results
The average BMD of the 7 specimens was 0.81±0.09 g/cm. The ROM of the three fixation constructs was significantly smaller than that of the intact group in all 6 directions (P < 0.05). In lateral bending, the ROM of groups 2 and 3 was significantly smaller than that of group 1 (P < 0.05), but groups 2 and 3 were not significantly different from each other (P >0.05). In flexion-extension, the ROM of groups 1 and 3 was significantly smaller than group 2 (P < 0.05), but groups 1 and 3 were not significantly different from each other (P >0.05). In axial rotation, the ROM of group 3 was significantly smaller than those of groups 1 and 2 (P < 0.05), but groups 1 and 2 were not significantly different from each other (P >0.05).
Conclusion
The four-rod technique achieved stable biomechanical effects in lumbosacral fixation. At the L5-S1 junction, the four-rod technique demonstrated better stability than the constructs using S1 screws or S1 screws plus iliac screws.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#稳定性#
36
#系统生物#
39
#Spine#
42