Cell Rep:治疗肌萎缩性脊髓侧索硬化症的新靶点MuSK
2012-09-10 T.Shen 生物谷
肌萎缩性脊髓侧索硬化症(ALS, Amyotrophic lateral sclerosis)是一种对大脑神经元和脊髓(控制随意肌移动)极具破坏性的进行性疾病。近日,来自纽约大学医学院的研究者发现了一种可以明显减缓由于该疾病引发的躯体功能衰退的靶点,相关的研究成果已刊登在国际杂志Cell Reports上。 平均1000人中有一人会发展成ALS,当前治疗该病的方法仅仅只是给病人带来舒适感,但是并

肌萎缩性脊髓侧索硬化症(ALS, Amyotrophic lateral sclerosis)是一种对大脑神经元和脊髓(控制随意肌移动)极具破坏性的进行性疾病。近日,来自纽约大学医学院的研究者发现了一种可以明显减缓由于该疾病引发的躯体功能衰退的靶点,相关的研究成果已刊登在国际杂志Cell Reports上。
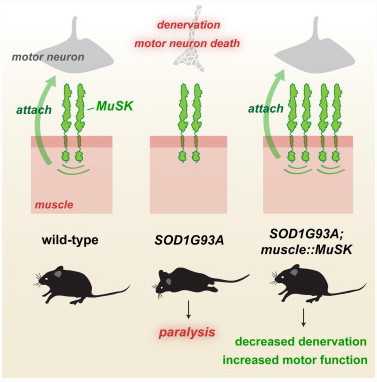
平均1000人中有一人会发展成ALS,当前治疗该病的方法仅仅只是给病人带来舒适感,但是并不能减缓疾病的发展过程。研究中,Steven J. Burden博士指出,通过增加骨骼肌受体酪氨酸蛋白激酶(muscle, skeletal receptor tyrosine-protein kinase,MuSK)的信号活性,可以ALS小鼠模型的神经细胞吸附在肌肉上。
高表达MuSK并不能延长ALS小鼠的寿命,尽管增加其表达,神经细胞最终依然会死。但是增加的MuSK信号可以保持神经元轴突和肌肉之间保持很长时间的“联系”,而这种联系对于从大脑到肌肉信号传导非常重要。
Burden教授的实验室在1993年发现了MuSK,而且一直重点研究该蛋白如何行使功能以及是否其活性可以被控制来影响疾病的发生。当前在小鼠的研究中研究者发现在出生小鼠中通过高表达MuSK可以使得小鼠发展为神经肌肉ALS症状。后期研究者将继续深入研究ALS症状发生后是否MuSK的水平会增加,这或许为治疗人类的ALS提供帮助。
编译自:Potential New Approach for Improving Quality of Life for Amyotrophic Lateral Sclerosis Patients

doi:10.1016/j.celrep.2012.08.004
PMC:
PMID:
Increasing MuSK Activity Delays Denervation and Improves Motor Function in ALS Mice
María J. Pérez-García, Steven J. Burden
Amyotrophic lateral sclerosis (ALS) is a devastating disease that progresses from detachment of motor nerve terminals to complete muscle paralysis and lethal respiratory failure within 5 years of diagnosis. Genetic studies have linked mutations in several genes to ALS, and mice bearing mutations in SOD1 recapitulate hallmark features of the disease. We investigated whether disease symptoms can be ameliorated by co-opting the retrograde signaling pathway that promotes attachment of nerve terminals to muscle. We crossed SOD1G93A mice with transgenic mice that express MuSK, a receptor tyrosine kinase that is required for retrograde signaling, and we used histological and behavioral assays to assess motor innervation and behavior. A 3-fold increase in MuSK expression delayed the onset and reduced the extent of muscle denervation, improving motor function for more than a month without altering survival. These findings suggest that increasing MuSK activity by pharmacological means has the potential to improve motor function in ALS.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#Cell#
29
#萎缩性#
41
#CEL#
24
#萎缩#
28
#硬化症#
25
#新靶点#
0
#肌萎缩#
38