Int J Cardiol:特发性肺动脉高压患者右心房功能与预后分析!
2017-08-24 xing.T MedSci原创
由此可见,该研究的数据表明RA功能在特发性PAH中具有预后价值,通过应变和SR分析得到的较差RA功能与更坏的结局相关。
近日,心血管领域权威杂志International Journal of Cardiology上发表了一篇研究文章,研究人员旨在明确右心房(RA)功能对特发性肺动脉高压(PAH)患者预后具有预测价值。
总体而言,104名(70名女性,平均年龄为58±13岁)特发性PAH患者在右心导管插入术前接受了标准的多普勒超声心动图和应变率(SR)分析。
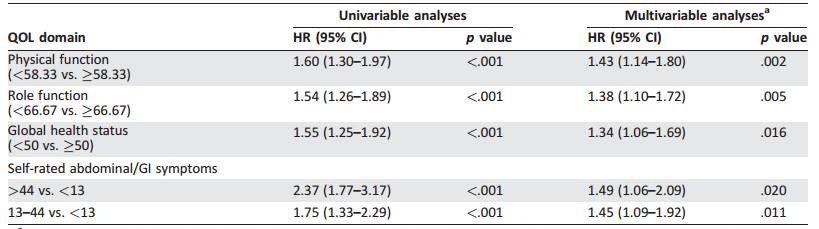
在平均22±7个月的随访中,30例(29%)患者出现临床恶化。在多变量Cox比例风险回归分析中,RA储器功能衡量指标有纵向SR峰值(风险比[HR]为0.5;P<0.0001)、RA面积(HR为1.2;P<0.01)、右室(RV)SR为(HR为0.6;P<0.0001)、心脏指数(HR为0.79;P<0.01)和混合静脉血氧饱和度(HR为0.82;P<0.01)被认为是心脏事件的独立相关因素。RA SR储器截断值<1.2s-1和RV SR截断值<1s-1能够很好地确定临床恶化风险更高的患者(灵敏度为85.5%;特异性为90.4%;检验准确度为88.8%)。特别是,事件的发生率和无临床恶化的平均生存时间:在正常RA和RV应变的患者分别为6.1%和23.5±2.2个月;在RA应变受损RV SR正常的患者分别为45%和20.9±5.5个月;在RV SR受损和RA应变正常的患者分别为56.2%和17.7±6.6个月;而RA应变和RV SR均受损的患者分别为87.5%和12.9±7.6个月。
由此可见,该研究的数据表明RA功能在特发性PAH中具有预后价值,通过应变和SR分析得到的较差RA功能与更坏的结局相关。
原始出处:
Michele D'Alto, et al. Right atrial function and prognosis in idiopathic pulmonary arterial hypertension.International Journal of Cardiology.2017. https://doi.org/10.1016/j.ijcard.2017.08.047
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#特发性肺动脉高压#
63
#特发性#
45
#Cardiol#
41
#右心房#
59
#动脉高压#
36
#肺动脉高压患者#
32
#心房#
31