Biomed Pharmacother:特立帕肽可促进新生血管形成
2017-12-06 MedSci MedSci原创
越来越多的研究表明,早期血管生成促进损伤的愈合。特立帕肽(PTH)因其对骨骼有效的合成代谢活性而得到了广泛的应用,但是关于其血管生成能力仍尚未可知。在这项研究中,我们测试了PTH和β-磷酸三钙降解(β- TCP)对股骨远端干骺端缺损去卵巢(OVX)大鼠血管生成能力的影响。成功建立了OVX模型后,在每只大鼠的股骨远端钻入一个临界尺寸缺陷。然后将所有的动物随机分为三组:对照组,β-TCP组和组β-TC
越来越多的研究表明,早期血管生成促进损伤的愈合。特立帕肽(PTH)因其对骨骼有效的合成代谢活性而得到了广泛的应用,但是关于其血管生成能力仍尚未可知。
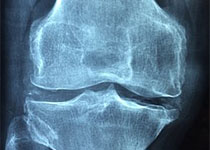
在这项研究中,我们测试了PTH和β-磷酸三钙降解(β- TCP)对股骨远端干骺端缺损去卵巢(OVX)大鼠血管生成能力的影响。成功建立了OVX模型后,在每只大鼠的股骨远端钻入一个临界尺寸缺陷。然后将所有的动物随机分为三组:对照组,β-TCP组和组β-TCP + PTH组,然后特立帕肽(30 μg/kg)每隔一天皮下注射βTCP + PTH。股骨手术后四周,每组五个标本探究血管形成情况。剩余大鼠进行显微CT、组织学及免疫组织化学检测。
结果表明,特立帕肽可促进新生血管形成和β-TCP降解,β-TCP存在下出现新骨形成,可能在早期阶段与新生血管相关。
原始出处:
Xie Z, Weng S, et al., Teriparatide promotes healing of critical size femur defect through accelerating angiogenesis and degradation of β-TCP in OVX osteoporotic rat model. Biomed Pharmacother. 2017 Nov 30. pii: S0753-3322(17)33816-7. doi: 10.1016/j.biopha.2017.11.141.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#新生血管#
26
#Bio#
32
#Pharm#
31
#pharma#
37
#MAC#
25
#特立帕肽#
38
#Med#
30
好好文章学习了
68