Nat Commun:从沙门氏菌获得灵感,攻克癌症耐药难题
2016-07-27 MedSci MedSci原创
在一项沙门氏菌试验中获得的惊人研究结果促成了一个研究发现,有可能使得传统化疗更容易治愈耐药癌细胞。麻省大学医学院的科学家们发现,沙门氏菌蛋白SipA可自然减少存在于许多不同类型癌细胞中的一种众所周知的耐药分子。通过传送附着这一蛋白的微型金纳米颗粒,研究人员可以大大提高肿瘤对一些化疗药物的敏感性,并缩小了小鼠体内的结肠癌和乳腺癌肿瘤。这项研究发布在7月25日的《自然通讯》(Nature Commun
在一项沙门氏菌试验中获得的惊人研究结果促成了一个研究发现,有可能使得传统化疗更容易治愈耐药癌细胞。麻省大学医学院的科学家们发现,沙门氏菌蛋白SipA可自然减少存在于许多不同类型癌细胞中的一种众所周知的耐药分子。通过传送附着这一蛋白的微型金纳米颗粒,研究人员可以大大提高肿瘤对一些化疗药物的敏感性,并缩小了小鼠体内的结肠癌和乳腺癌肿瘤。这项研究发布在7月25日的《自然通讯》(Nature Communications)杂志上。
麻省大学医学院微生物学与生理系统教授与副主任Beth A. McCormick博士,和生物化学与分子药理学助理教授、纳米医学专家韩纲(Gang Han)博士是这篇论文的共同通讯作者。
McCormick说:“考虑到研究发现有着惊人的临床潜力来治疗某些耐药癌症,这是一件很有意思的事情。基于这些研究结果,我们已经进入到临床前开发阶段。”
在150多年里,科学家们观察到各种类型的细菌可以减少癌肿瘤。最近,调查人员提出利用沙门氏菌一类的细菌可以直接刺激对抗癌细胞的免疫反应。研究人员还发现一些细菌可以选择性地在肿瘤中生长,表明有其他的治疗潜力。尽管获得了这些观察发现,对于控制这些不同效应的机制仍不清楚。由于与免疫相关反应相关的一些原因以及出于对潜在感染的担心,一些利用沙门氏菌或其他细菌进行治疗的尝试也未取得成功。
作为传染病专家,McCormick博士调查了沙门氏菌利用来攻克细胞的天然防御以感染它们的生物学工具。具体地说,她检测了SipA对于人类肠细胞上某些转运蛋白的影响。认为SipA有可能上调了其中的一个蛋白诱导了炎症反应,McCormick利用一种常见转运蛋白P-gp作为对照完成了一系列的实验。并未指望找到什么不同寻常的东西,然而她却获得了惊人的研究发现:这一细菌产物几乎完全清除了P-gp转运蛋白。
存在于细胞表面的P-gp通常负责清除废物,将异物、碎片和毒素泵出细胞外。出于这一原因,McCormick认为沙门氏菌需要让P-gp蛋白丧失功能,因此它能够更容易地感染细胞。在癌症复发的情况下,肿瘤细胞中过度丰富的P-gp可导致形成耐药性。在这些细胞中,P-gp发挥作用在化疗和抗癌药物累积并杀死细胞之前将它们泵出细胞外。McCormick想知道P-gp对于癌症耐药的重要性。这一新证据表明,仅SipA就可以除掉对多药耐药癌症负责的P-gp蛋白。
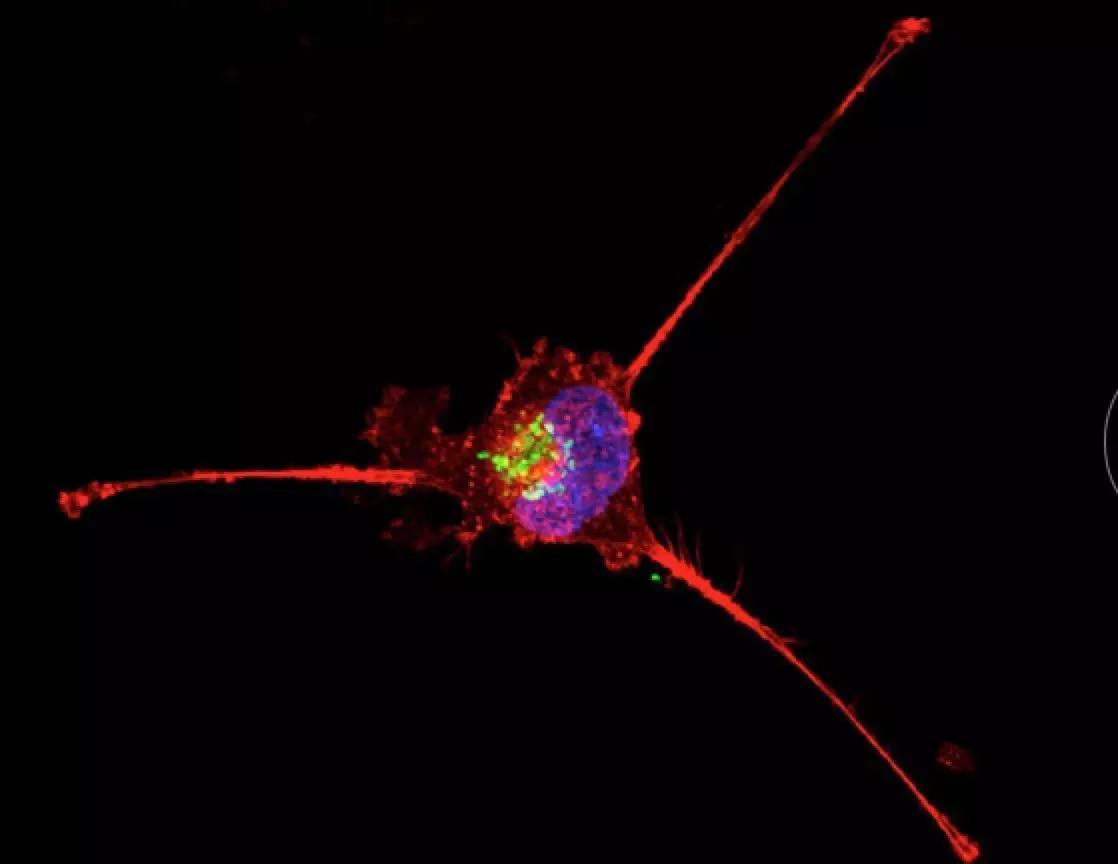
尽管SipA有潜力用作抗癌治疗,仍然必须将这一蛋白传递到体内的肿瘤处。McCormick与韩纲合作开发了一种携带SipA的沙门氏菌纳米颗粒模拟物。韩纲说:“在细菌外,SipA蛋白极不稳定无法简单地注射到潜在患者体内。并非利用整个细菌,我们开发了一种纳米颗粒支架来模拟细菌,稳定并传递这一蛋白。我们将这一颗粒称作为‘纳米菌’(nanobug)。”
由于它的惰性和独特的三维支架,韩纲选择黄金开发出了一种纳米颗粒,其小至可以渗入肿瘤,又大至无法被大多数的生物组织吸收。论文的第一作者、McCormick实验室博士后Regino Mercado-Lubo说:“肿瘤不同于正常组织。它们往往渗透,因此我们希望我们的纳米菌能够渗入肿瘤且不在其他组织中累积。”
研究人员在一个结肠癌小鼠模型和一个人源化乳腺癌小鼠模型中采用了SipA-nanobug和广泛使用的化疗药物阿霉素(Doxorubicin)。Mercado-Lubo说:“结果是惊人的。在30天几乎检测不到肿瘤。这是不同寻常的。在某些情况下,肿瘤变得比组织薄切片还要小。”
根据Mercado-Lub所说,同样重要地是,没有金纳米颗粒在肺、心脏或脑组织中累积。
下一步,McCormick、韩纲和同事们将进一步推动研究进入临床前开发。这将帮助确定推动这一纳米菌进入患者试验的安全性、毒性和剂量水平。
McCormick说:“近20年来,科学家们一直希望通过筛查成千上万的小分子寻找P-gp抑制剂来逆转癌细胞耐药。这些尝试都未能转化至临床。有了SipA我们获得了自然的优先权和200万年的共进化,表明它可以有效地除去细胞中的P-gp,且不会诱导免疫反应。”

韩纲说:“我们开发的这一细菌纳米颗粒模拟物有潜力稳定一些治疗蛋白,与广泛的临床化疗药物联合使用来克服多种肿瘤中的多药耐药。”
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Nat#
30
#COMMUN#
27
长见识了
64
#癌症耐药#
29
#沙门氏菌#
37
继续学习
86