O药 vs. K药论剑华山,11种癌症临床研究数据对比
2018-08-21 医药魔方 医药魔方
默沙东KEYTRUDA(K药)和百时美施贵宝OPDIVO(O药)终于都成功在中国上市了,这让不少肿瘤患者看到了希望。 O药 、K药基本信息 俗称 O药 K药
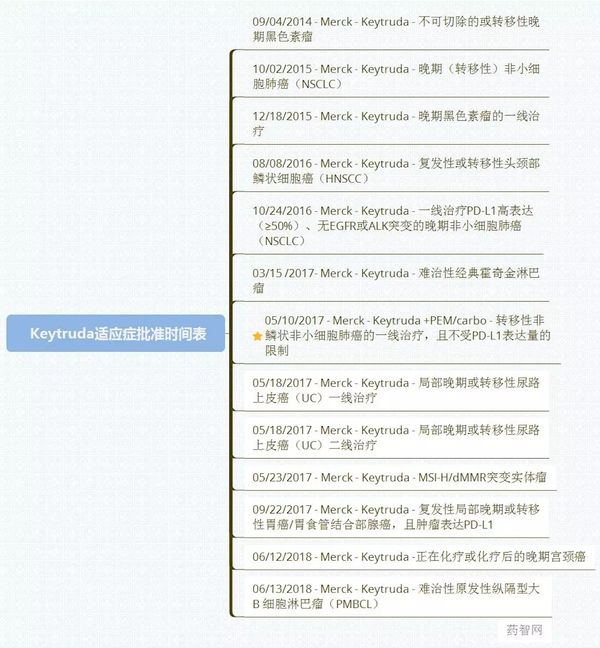
默沙东KEYTRUDA(K药)和百时美施贵宝OPDIVO(O药)终于都成功在中国上市了,这让不少肿瘤患者看到了希望。 O药 、K药基本信息 俗称 O药 K药 商品名(英文) Opdivo Keytruda 商品名(中文) 欧狄沃 可瑞达 通用名(英文) Nivolumab Pembrolizumab 通用名(中文) 纳武单抗 派姆单抗 帕博利珠单抗 这么多名称,连从事医药工作的小编都看的懵逼,特别强调一下,帕博利珠单抗就是派姆单抗,并不是新出的另外一种,看到以上名称时请根据表格内自行对号入座。 O药 、K药的适应症 O药和K药目前所批的适应症均包括9-10种癌症: 编号 O药 K药 1 黑色素瘤 黑色素瘤 2 非小细胞肺癌 非小细胞肺癌 3 霍奇金淋巴瘤 霍奇金淋巴瘤 4 膀胱癌 膀胱癌 5 头颈部鳞状细胞癌 头颈部鳞状细胞癌 6 结直肠癌 高度卫星不稳定性实体瘤 结直肠癌 小肠肿瘤 肉瘤 子宫内膜癌 乳腺癌 甲状腺癌 胆管癌 膀胱癌 腹膜后腺癌 胃癌 食管癌 小细胞肺癌 胰腺癌 前列腺癌 肾细胞癌 7 肝癌 大B细胞淋巴瘤 8 肾癌 胃癌 9 尿路上皮癌 子宫颈癌 10 尿路上皮癌
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#研究数据#
40
学习了感谢分享
79
好
86
#O药#
39
#K药#
45
学习学习很好
61
谢谢分享,学习了
83
了解一下谢谢
67
嗯嗯,学习了。
20