Int J Radiat Oncol Biol Phys:颅咽管瘤手术术后辅以质子治疗有益于患者预后
2021-06-27 MedSci原创 MedSci原创
颅咽管瘤患者在接受质子治疗前低于平均水平的神经认知表现与白质结构完整性的整体退化有关,这部分归因于手术、梗阻性脑积水或术前下丘脑受累。
颅咽管瘤约占儿童脑和中枢神经系统肿瘤的4%。尽管颅咽管瘤的总生存率很高(5年83%-96%),但生存者经常经历神经认知障碍和其他后遗症,如下丘脑功能障碍和内分泌缺陷,为了降低潜在的手术发病率,流行的治疗策略之一是手术后辅以辅助质子治疗。由于质子治疗在保留与临床结果相关的大脑结构方面的剂量优势,人们越来越多地认为质子治疗可以取代光子治疗。先前的研究表明,儿童颅咽管瘤患者接受质子治疗后,早期毒性表现良好,病情控制满意。然而,由于这种疾病的罕见性和质子治疗的出现相对较晚,我们对治疗相关结果的理解有限,特别是在治疗相关的正常大脑损伤及其对神经认知功能的影响方面。
Int J Radiat Oncol Biol Phys.杂志最近刊发文章,研究儿童颅咽管瘤接受质子治疗后,脑白质完整性与神经认知功能的照射前基线相关性,并评估治疗后的变化。

该研究分析了照射前基线的神经认知数据,以确定与DTI测量的联系,考虑了全脑手术的影响和其他临床因素。纵向DTI分析包括了更多的患者和更长的随访时间,并使用了先进的方法(TBSS、结构连接学)来检查整个白质束,而不局限于先验确定的感兴趣区域。
这项前瞻性治疗试验中,90例儿童和青少年(2-20岁)颅咽管瘤采用质子治疗(54gy [RBE])。分析质子治疗前的术后基线神经认知表现以及基线和年度随访时获得的弥散张量成像(DTI)数据。基于区域的空间统计和结构连接组学用于从DTI中获得整体和局部白质特征。比较平均和低于平均神经认知能力患者的基线DTI特征。研究人员对纵向DTI数据进行分析,以确定质子剂量对脑白质结构的影响与受照脑容量和基线年龄有关。
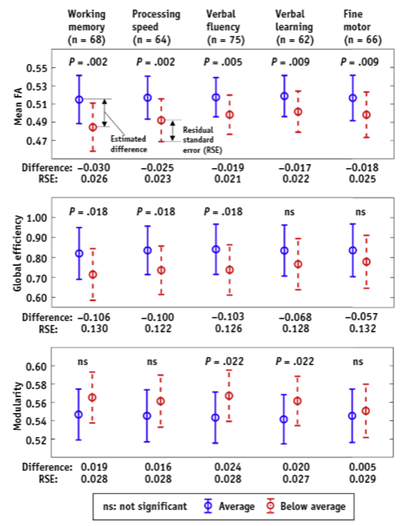
通过分析神经认知能力低于平均水平和平均水平的患者的协方差来比较DTI测量。给出了各组中位年龄(9岁)的DTI估计值,误差线代表RSE。所有值均被错误发现率纠正。除了表现是否低于平均水平外,基线年龄和性别也作为协变量。在估计的差异之前的负号表明,表现低于平均水平的组的DTI测量值较小。
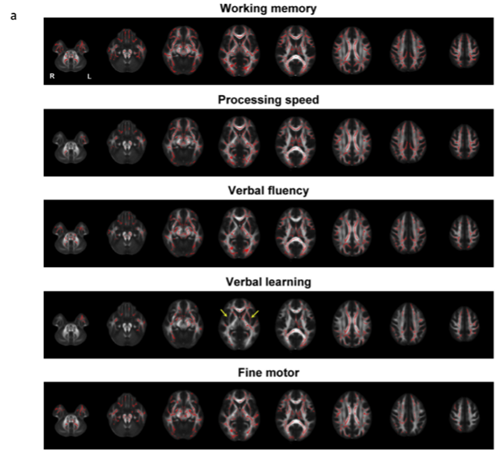
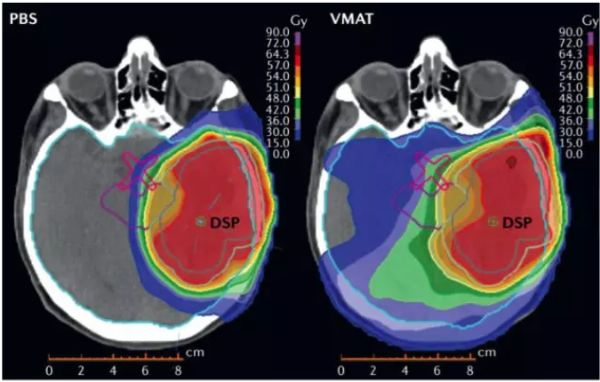
基线TBSS分析的结果与手术和放射的空间信息相比较。(a)白质骨架体素(以红色突出显示)在神经认知表现低于平均水平的患者中表现出明显低于平均水平的患者。用于语言学习的图像中的箭头表示与内外囊的左偏关联。(b)根据与每项神经认知功能显著相关的骨骼体素的百分比,比较左、右白质束。(c)手术缺陷占位频数图。色标代表所分析患者总数的百分比(nZ90)。(d)所有患者的平均质子剂量分布。色标以Gy(RBE)为单位表示剂量。
在质子治疗前,工作记忆、处理速度、语言流畅性、语言学习或精细运动灵活性低于平均水平的患者与表现一般的患者相比,白质结构整体退化更多,表现为平均分数各向异性较低、整体效率降低或模块化程度较高。手术、梗阻性脑积水和术前下丘脑受累似乎与这种退化有关。

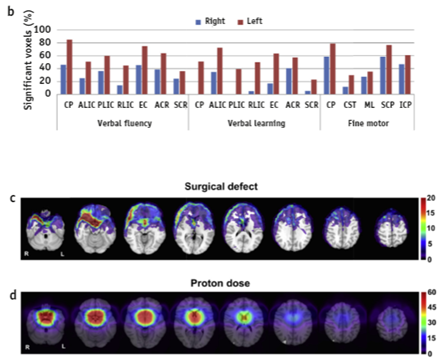
质子治疗(PT)后全脑DTI测量的纵向趋势由GEE模型确定(n=89,排除1例仅有基线DTI的患者)。多维回归的二维图要求指定图中不包括的回归子。(a)中位基线年龄(9岁)和中位照射脑体积图(V90brain =2.5%)。在每种情况下,中心线表示回归,阴影带代表95%的置信区间。β是GEE的时间项系数。(b)为了证明受照射脑体积对纵向趋势的影响,将受照射脑体积的下四分位数和上四分位数(V90brian,分别为1.8%和3.6%)与基线年龄中位数进行对比。这些值表明了时间与照射脑体积之间相互作用项的意义。(c)基线年龄对上四分位数和下四分位数(分别为6岁和13岁)以及中值受照射脑容量的影响同样得到证明。
在局部分析中,基于束的空间统计显示左偏侧与语言和运动功能相关,这支持通过右半球手术治疗中线肿瘤。在质子治疗后的5年里,大脑的平均各向异性分数和DTI的整体效率都增加了。照射脑体积和儿童年龄越大,FA和整体效率增长速度越低。
颅咽管瘤患者在接受质子治疗前低于平均水平的神经认知表现与白质结构完整性的整体退化有关,这部分归因于手术、梗阻性脑积水或术前下丘脑受累。语言和优势手精细运动功能与大脑左侧相关白质束的关联关系支持右侧手术入路的使用。质子治疗后5年,DTI完整性和效率的总体改善趋势,尤其是在受照射脑体积较小的儿童中,这与新出现的文献表明质子治疗后认知结果稳定一致。
原文出处
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Oncol#
36
#Biol#
46
#DIA#
35
#患者预后#
42
#Bio#
35
#质子治疗#
33
#颅咽管瘤#
44
谢谢梅斯分享这么多精彩信息
41