PD-L1免疫疗法Durvalumab治疗NSCLC喜获FDA突破性药物资格
2017-08-10 放瘤娃 肿瘤资讯
Durvalumab上市后,市场上就一共有五种抗PD-1/L1的药物,那么此次其在非小细胞肺癌上获得的突破性药物资格,FDA的依据是什么?突破性药物资格又意味着什么?
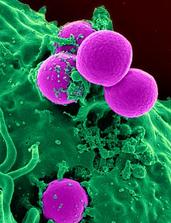
近日,Durvalumab 获得美国食品药品监督局(FDA)突破性的药物资格,其为抗PD-L1的单克隆抗体,目前用于局部晚期不可手术的非小细胞肺癌(NSCLC)患者,在进行以铂类药物为基础的治疗后,疾病不再进展后的维持治疗探索。
目前,Durvalumab用于局部晚期不可手术的非小细胞肺癌的治疗尚未获得FDA批准。
本次Durvalumab 所获得的突破性药物资格,FDA依据的是PACIFIC的III期临床研究的中期结果,这是一个双盲,以安慰剂为对照组的多中心研究,研究目的为局部晚期不可手术的非小细胞肺癌患者(III期),在进行以铂类为基础的同步放化疗后,疾病无进展时以Durvalumab作为后续治疗药物的探索。PACIFIC临床研究的数据将在即将举行的医学会议上发表。
在2017年5月,Durvalumab获得了FDA批准用于局部晚期或转移性尿路上皮癌的治疗,这部分患者在使用包含铂类药物的化疗后疾病出现进展,或在术前或术后接受含铂药物化疗的12个月内疾病出现进展。对于这一适应症,FDA依据肿瘤的反应率及持续反应的时间,将Durvalumab纳入加速批准流程后,予以批准用于治疗。
而对于NSCLC这一适应症的批准,后续可能还会依据临床试验中患者获益的描述和验证。
点评
在PACIFIC的III期研究中,针对的对象是局部晚期不可手术的非小细胞肺癌,且在含铂方案同步放化疗后无进展。也就是说,从无进展到肿瘤进展,存在一个窗口期。在这个窗口期中,除了肿瘤原发灶外,同步放化疗方案中放疗的常规分割,也在一定程度上会促进PD-1在T细胞上的表达,Durvalumab正好应时而生,虽然目前难以做到OS的大获全胜,但能延长PFS,也是小胜。
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#药物资格#
0
#mAb#
32
#突破性药物资格#
41
#突破性药物#
43
#PD-L1#
34
在PACIFIC的III期研究中,针对的对象是局部晚期不可手术的非小细胞肺癌,且在含铂方案同步放化疗后无进展。也就是说,从无进展到肿瘤进展,存在一个窗口期。在这个窗口期中,除了肿瘤原发灶外,同步放化疗方案中放疗的常规分割,也在一定程度上会促进PD-1在T细胞上的表达,Durvalumab正好应时而生,虽然目前难以做到OS的大获全胜,但能延长PFS,也是小胜。
47
Durvalumab获得美国食品药品监督局(FDA)突破性的药物资格,其为抗PD-L1的单克隆抗体,目前用于局部晚期不可手术的非小细胞肺癌(NSCLC)患者,在进行以铂类药物为基础的治疗后,疾病不再进展后的维持治疗探索。
40
学习
42
学了。。。。。。。。。。
43
学习学习
47