BMC Cancer:多中心数据探索nivolumab治疗经治转移性胃癌患者获益的临床预后因素
2022-01-10 yd2015 MedSci原创
研究表明,nivolumab可能对身体状态差和有曲妥珠单抗治疗史的患者AGC无效。
尽管nivolumab(PD-1抑制剂)是一种有前途的治疗晚期胃癌(AGC)的方法,但其疗效仍然有限。来自日本的学者开展了相关回顾性多中心研究,目的是确定nivolumab治疗经治转移性胃癌患者获益的临床预后因素。相关结果发表在BMC Cancer杂志上。

从2017年10月到2018年12月,纳入58例患者。58例患者包括45名男性(78%)和13名女性(22%)。Nivolumab开始使用时的中位年龄为66岁(范围,3882岁)。8例(14%)患者的ECOG PS为0,50例(86%)患者的ECOG PS≥1。诊断时,43例(74%)患者被归类为转移性,15例(26%)复发。
在接受nivolumab治疗的58例患者中,没有患者达到CR,4例患者达到PR(7%), 17例患者达到SD(29%),其余37例患者PD(64%),因此ORR为7%,疾病控制率(DCR)为36%。
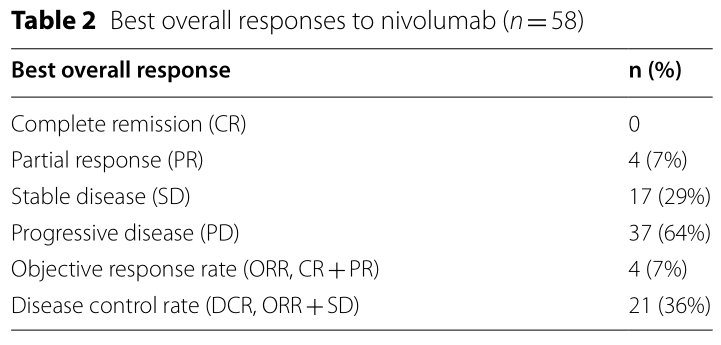
疗效评估
DCR明显跟ECOG PS=0 (p = 0.021),一个器官转移灶(p = 0.006)和≥2级irAE(p=0.027)相关。
31例(53%)患者经历了TRAE;18例(31%)患者为2级或以上。最常见的TRAE为厌食症(n = 9)、乏力(n = 6)和恶心(n = 3)。
中位OS为5.95个月(95% CI 4.2-7.7),中位PFS为1.6个月(95% CI 1.4-2.6)。有应答者的中位OS未达到(95% CI 8.0-NA),无应答者的中位OS为3.8个月(95% CI 2.3-5.1) (p<0.0001)。有应答者的中位PFS为6.1个月(95% CI 4.0-11.0),无应答者的中位PFS为1.4个月(95% CI 1.2-1.4) (p<0.0001)。

PFS和OS
Nivolumab治疗后进展后,接受化疗组的中位OS为9.7个月(95% CI 6.3-17.8),未接受化疗组的中位OS为2.9个月(95% CI 1.9-4.4) (p<0.0001)。
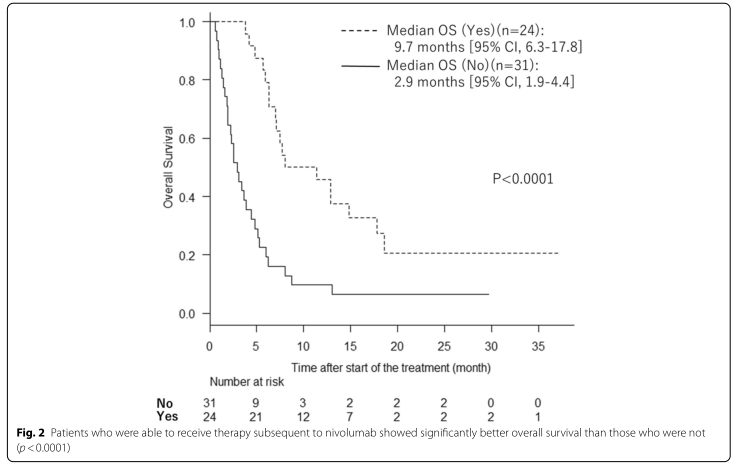
后续有无化疗的OS差异
在Cox比例风险回归模型中,以下变量被确定为与不良预后显著相关:ECOG PS ≥1 (p = 0.018),既往使用曲妥珠单抗治疗(p = 0.040),无irAEs (p = 0.017),对nivolumab无反应(p <0.001),以及无法接受后续化疗(p<0.001)。除了对nivolumab无反应外,没有变量与无进展生存期显著相关。
综上,研究表明,nivolumab可能对身体状态差和有曲妥珠单抗治疗史的患者AGC无效。
原始出处:
Sano A, Sohda M, Nakazawa N, Ubukata Y, Kuriyama K, Kimura A, Kogure N, Hosaka H, Naganuma A, Sekiguchi M, Saito K, Ogata K, Sakai M, Ogawa H, Shirabe K, Saeki H. Clinical features as potential prognostic factors in patients treated with nivolumab for highly pretreated metastatic gastric cancer: a multicenter retrospective study. BMC Cancer. 2022 Jan 3;22(1):22. doi: 10.1186/s12885-021-09118-3. PMID: 34980017; PMCID: PMC8721909.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#BMC#
33
#多中心#
41
#转移性胃癌#
46
#mAb#
37
#胃癌患者#
46
#NIV#
29
学习
44
#转移性#
27
#预后因素#
30
#临床预后#
42