“双重磅”突破性临床研究成果发布,为糖尿病治疗提供新选择
2021-08-24 梅斯医学 梅斯医学
2021年8月24日,第81届美国糖尿病学会(ADA)学术年会于6月底落下帷幕,众多糖尿病领域的临床研究项目在会上公布了最新进展和成果。
2021年8月24日,第81届美国糖尿病学会(ADA)学术年会于6月底落下帷幕,众多糖尿病领域的临床研究项目在会上公布了最新进展和成果。借此契机,自7月开始,赛诺菲在全国十余个城市巡回举办了2021 BEYOND-ADA 高级学术研讨会(以下简称“研讨会”),邀请众多糖尿病领域专家和临床医生参与,就糖尿病临床治疗及低血糖预防等全球研究进展进行了分享和探讨。同时,通过生动形象的视频,对专业知识进行解读,与广大专业医生分享。其中,赛诺菲在今年ADA年会上公布的两项关键研究——SoliMix及BEYOND V的结果成为了重点讨论的对象。
SoliMix:为使用预混胰岛素的患者提供新选择
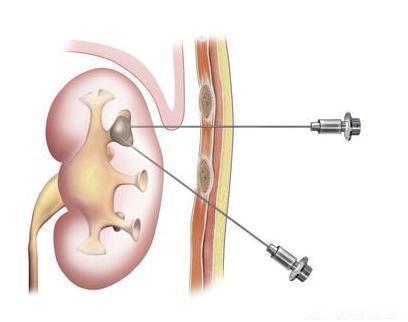
预混胰岛素在中国应用广泛,约有半数以上的中国2型糖尿病患者接受胰岛素治疗时使用预混胰岛素i,尽管预混胰岛素被认为是一种较为普遍的治疗选择,其在临床应用中仍然存在明显的低血糖风险和体重增加的问题ii。
此次研讨会就ADA大会上公布的首个比较基础胰岛素与GLP-1RA的复方制剂(iGlarLixi*)与预混胰岛素的头对头研究——SoliMix进行了分享和探讨。SoliMix研究结果显示,iGlarLixi的疗效优于预混胰岛素,且明显降低体重。同时,iGlarLixi还具有空腹血糖控制更优、胰岛素剂量更少、低血糖风险更低等优势iii。此外,在治疗负担、日常生活、糖尿病管理、患者依从性、心理健康及治疗效果等多个维度,iGlarLixi的患者报告结局都优于预混胰岛素iv。
中日友好医院内分泌科杨文英教授接受采访时表示:“ADA的会后会让我们在新疫情时代仍旧能及时了解到国际上对于创新药物研发的最前沿进展,例如SoliMix研究。其成果表明了每日一次注射的iGlarLixi相较于每日两次注射的预混胰岛素具有更优的安全性及疗效,同时,其注射量更少,血糖监测更少的优势可以帮助广大临床医生优化当下的复杂胰岛素治疗方案,进一步提升患者的依从性。” 另外, iGlarLixi在中国也开展并顺利完成了三期临床研究, 其中,LixiLan-O AP研究由杨文英教授牵头, 针对口服药控制不佳的患者将iGlarLixi对其组分单药治疗进行了对比试验,杨教授表示:“基础胰岛素通过降低空腹血糖带动实现整体血糖正常化,部分患者可能仍有控制餐后血糖的需求,在这样的状况下,其另一组分利司那肽能发挥其效用,总体来说,iGlarLixi为口服药控制不佳的患者都提供了一种全面降糖的简便方案,且这种方案能基本解决患者对目前降糖药物未满的需求,我们非常期待中国三期研究的正式发布。”
BEYOND V:探索短期住院强化后胰岛素治疗方案的选择
据统计,中国有近50%的糖尿病患者在住院期间接受起始胰岛素治疗v,这类患者主要因高血糖住院,首要治疗目标是控制高血糖、改善高糖毒性。目前,短期的住院胰岛素强化治疗是针对这类患者的主要治疗方法,但是患者在出院后如何选择合适的治疗方案,仍是临床上待解决的问题。
在这一背景下,北京医院内分泌科主任郭立新教授及解放军总医院内分泌科主任母义明教授牵头开展了BEYOND V研究,在口服降糖药控制不佳且接受过短期胰岛素强化治疗的2型糖尿病患者中,对比了每日一次的甘精胰岛素U100联合口服降糖药和每日两次的预混胰岛素(双相门冬胰岛素30,BIAsp30)联合口服降糖药的疗效和安全性。
北京医院内分泌科主任郭立新教授接受采访时表示:“短期胰岛素强化治疗后,中国2型糖尿病患者长期维持方案有着诸多选择,而此次BEYOND V研究为患者在强化胰岛素治疗后胰岛素治疗方案选择方面提供了有力证据。结果表明,短期胰岛素强化治疗后,相较于预混胰岛素(门冬胰岛素30,BIAsp30)联合口服降糖药的治疗方案,甘精胰岛素U100联合口服降糖药的治疗方案显示出相当的疗效,但其低血糖发生风险更低、安全达标率更高、胰岛素使用剂量更少。”此外,针对短期胰岛素强化治疗,郭教授表示:“目前临床上比较推崇的是采用‘先基础后餐时’的治疗方案,它也是最符合我们生理性胰岛素分泌规律的方案。其优势体现在可有效促进血糖快速达标、治疗期间低血糖风险较低且无严重低血糖发生、剂量调整方便、操作简便以及患者依从性更好等方面。同时,我们也期待这样一个源自于中国的研究,能够为中国更多的临床医生及糖尿病患者带来治疗方面的启示。”
赛诺菲大中华区普药医学部负责人谷成明博士表示:“自进入中国以来,赛诺菲始终致力于改变中国糖尿病患者的生存现状,专注患者未被满足的治疗需求,未来我们将持续引领糖尿病领域的创新突破,帮助患者减轻身心负担,获得高质量的生活。”
* iGlarLixi是一种注射类降糖药,由甘精胰岛素100U/mL与利司那肽按固定比例组合而成。iGlarLixi尚未在中国获批。iGlarLixi在欧盟被称为“Suliqua®”,Suliqua®可用于联合生活方式管理及二甲双胍或二甲双胍和SGLT2抑制剂,改善成人2型糖尿病患者的血糖控制情况;iGlarLixi在美国被称为“Soliqua®100/33”,可联合生活方式管理用于改善成人2型糖尿病患者的血糖控制情况;在其他获批地区,iGlarLixi也被称为“Soliqua®”。
参考资料
i Polinski JM, et al. BMC Endocr Disord 2015;15:46;
ii Meece J Diabetes Ther 2018;9:877–90
iii Rosenstock, Julio et al. Diabetes Care. 2021 Jun 28;dc210393.
iv 2021 ADA ePoster 747 P-Improved Treatment Perceptions with iGlarLixi vs Premix Insulin in Type 2 Diabetes (T2D) Uncontrolled on Basal Insulin (BI) + Oral Antihyperglycemic Drugs (OADs): Patient-reported Outcomes (PROs) of the SoliMix Trial
v Liu, Jing, et al. Advances in therapy 37.4 (2020): 1675-1687.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#研究成果#
46
#糖尿病治疗#
45
#临床研究成果#
37
#重磅#
34
谢谢MedSci提供最新的资讯
52
学习了
63
双重压
58