
支架内再狭窄病变
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言

对复杂冠状动脉病变进行冠状动脉介入时,使用血管内超声显像 (IVUS) 可以得到更好的临床结局。不过有数据表明,当使用药物洗脱支架治疗时,IVUS的临床应用就会受到限制。研究者进行了一项研究,探究长冠状动脉病变(植入支架长度 ≥28 mm)患者进行药物洗脱支架植入时,通过IVUS能否更优于血管造影术。该随机多中心研究纳入了1400名患者,使用依维莫司涂层支架植入时,随机使用IVUS(n=700)或
冠状动脉疾病患者接受药物涂层的金属支架后,因为冠脉内金属的持续存在,可能会导致靶病变血管治疗的失败。而生物可吸收支架或许可以取代金属支架,获得更好的长期预后。研究者进行了一项大型、多中心、随机试验,纳入2008名稳定或不稳定心绞痛患者, 按2:1分为依维莫司涂层的可吸收性生物支架(Absorb n=1322)和依维莫司涂层的钴-铬金属支架(Xience n=686)。靶病变血管治疗失败包括心脏死亡
高出血风险患者接受经皮冠状动脉介入术(PCI)后会进行为期1个月的双重抗血小板治疗。该研究的目的是探究对于接受PCI术后进行一个月双重抗血小板治疗的高危出血患者,裸金属支架和佐他莫司洗脱支架植入后对机体的影响。
依维莫司洗脱生物可吸收血管支架(BVS)是为了与金属药物洗脱支架在1年时有可比性结果而设计的,以改善长期预后。无论BVS的1年的临床和血管造影结果劣于当前代药物洗脱支架的证据还尚未建立。中国使用已经批准的BVS一项随机试验中,旨在评估BVS的造影效果和BVS的临床安全性和有效性。符合条件的患者有1或2个的原发冠状动脉病变患者以1:1的比例随机分配接受BVS或钴铬依维莫司洗脱支架(CoCr-EES)
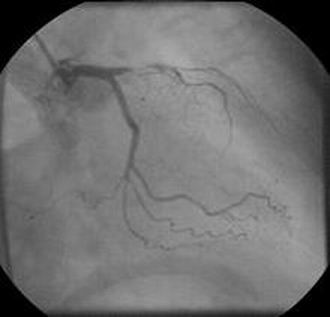
女性,22岁,以往因患有原发性肺动脉高压病左主冠状动脉植入血管支架,目前支架发生移位,迁移至主动脉(如图A)。随即,该女士被送往医院肺移植中心评估诊断。


梅斯医学MedSci APP
医路相伴,成就大医
#支架内再狭窄#
39
好文章,值得收藏
150
#再狭窄#
46