近年Barrett食管研究进展,要点来了!
2020-04-01 寒轻梅瘦 医学之声
胃食管反流一个常见和潜在的严重后果,是食管下段的鳞状上皮被柱状上皮所取代,这一状况被称为Barrett食管(BE)。
胃食管反流一个常见和潜在的严重后果,是食管下段的鳞状上皮被柱状上皮所取代,这一状况被称为Barrett食管(BE)。
BE最受关注的问题是增加食管腺癌发病风险,当BE伴有异型增生时癌变率更高。
2017年中国巴雷特食管及其早期腺癌筛查与诊治共识(以下简称共识)建议,BE食管<3cm伴有肠上皮化生者,建议每3~5年行1次内镜检查;对于BE≥3cm者,建议每2~3年行1次内镜检查。
病因与症状
BE病因未明,临床上多继发于胃食管反流,反流成分包括胃液、胆汁、胰液等可引起鳞状上皮受损,由耐酸的柱状上皮进行修复,从而形成BE。
此外,2017年发表于Clin Gastroenterol Hepatol的荟萃分析显示,年龄增加、男性、吸烟、较长的BE节段和低度异型增生都预测巴雷特食管的进展。
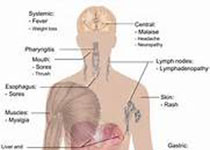
BE本身并不产生症状,症状主要由于反流性食管炎及其伴随病变引起,包括反酸、胃灼热、胸骨后疼痛、上腹痛、咽下困难、烧心等。
检查、诊断与分型
X线较难发现BE,BE的诊断必须要有内镜和组织病理学依据。
内镜下表现为食管远端胃食管交界上方灰白色食管鳞状上皮处出现橘红色,伴(或)有栅栏样血管表现的柱状上皮区域,柱状上皮区呈天鹅绒样,按形态可分为全周型、舌型和岛状,按化生长度可分为≥3 cm的长段和<3 cm的短段。
病理化生上皮分为胃底型、贲门型、肠化型,异型增生分为腺瘤样和小凹型。腺瘤样细胞形成腺管或绒毛状结构,细胞质红染,腺腔缘锐利,可见杯状细胞和潘氏细胞,MUC2、CDX-2和Villin呈阳性;
小凹型细胞呈立方或柱状,细胞质透明,腺腔缘不太清楚,无杯状细胞和潘氏细胞,MUC2、CDX-2和Villin均为阴性。
治疗
1.药物治疗
共识意见,BE伴有糜烂性食管炎以及反流症状者,建议应用大剂量抑酸剂治疗,可辅以黏膜保护剂、促动力药等。
抑酸剂主要是质子泵抑制剂(PPI)和组胺H2受体拮抗剂(H2RA)。
2018年,M.C.Tan,H.B.El-Serag等在巢式病例对照研究中观察到,与非使用者相比,PPI使用者从BE到腺癌的进展风险降低40%以上,H2RA使用者从BE到腺癌的进展风险降低30%。
单剂量PPI治疗无效时可改为双倍剂量(早餐和晚餐前分2次服用);一种PPI无效可改用另一种PPI。
促动力药:如多潘立酮、莫沙必利,可促进胃肠排空,减少酸反流。黏膜保护剂:如铋剂、铝碳酸镁等,可加强黏膜防御功能。
非甾体抗炎药:如阿司匹林,可通过抑制环氧合酶2,使腺癌的风险降低32%。
2018年,发表在The Lancet一项研究涵盖85个研究中心的大型随机临床试验,发现对于BE患者来说,在使用PPI治疗的同时,给予阿司匹林可能会带来额外的获益,虽然阿司匹林可能增加消化道出血等风险,但是大剂量PPI足以使风险降至可接受范围。
他汀类药物:可使BE进展为腺癌的风险降低。
同样是2017年Clin Gastroenterol Hepatol荟萃分析,发现使用他汀的患者BE进展的风险较低(OR=0.48;95%CI,0.31-0.73),有希望用于化学预防,但还需要更多的研究。
2.内镜治疗
2018年,Gastrointest Endosc提供了关于对BE进行内镜根除治疗(EET)的最具体建议,对BE中任何级别的不典型增生和黏膜内癌,推荐统一实施EET,对黏膜内癌推荐首选内镜而非手术,所有可见病变都应在EET前切除。
EET包括射频消融(RFA)、内镜下黏膜切除术(EMR)等。对重度异型增生的BE首选EMR或手术治疗。
RFA治疗BE的主要原理,是采用高频射频波破坏食管的内皮细胞,使得食管内皮的异常细胞或癌前细胞被破坏,原本位置上正常的组织可以再生修复。
BE消融治疗复发是常见的,内镜监测提供了治疗复发的可能。
2019年,发表于Gut的前瞻性分析发现,BE患者RFA治疗症状缓解后,复发风险在头5年中基本稳定,可适当延长复查频率,在复查中胃食管结合部取样活检十分重要。
结合2016年发表在Gastroenterology的研究,在BE柱状上皮化生<1cm的患者中,高度不典型增生或食管腺癌进展风险极低。
对于Z线不规则患者,不用进行活检,即使发现肠化生,最初5年进展风险仍不存在,随访监测内镜很可能不需要。
3. 外科治疗
手术治疗适用于BE伴严重的症状性反流,内科治疗无效者。最常见的方式是Nissen胃底折叠术,通过重建胃食管交界部的抗反流活瓣,达到抑制反流防止柱状上皮继续发展和向上扩的目的。
2018年,AOE杂志分享了塞尔维亚临床中心消化外科Ognjan M. Skrobi?等所着Concurrent radiofrequency ablation and Nissen fundoplication,提到:
Nissen胃底折叠术在部分RFA患者中可能具有重要作用,尤其是对食管远端有严重解剖损伤的患者。RFA作为并行的治疗方法,可能有助于降低BE患者的早期复发率。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













学习了~
50
学习了
52
好文
40
#RET#
32
#研究进展#
35
#Barrett食管#
43
#食管#
28
#Barrett#
35