Eur Heart J-Card Img:急性心力衰竭三尖瓣反流!
2018-02-11 xing.T MedSci原创
由此可见,伴有症状性HF和显著TR的患者存在多种并存的心脏异常。TR在正常或轻度升高的肺动脉压力的患者中TR并没有增加额外的风险。但是,它与PH患者的再住院和死亡率相关。
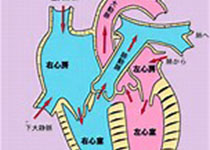
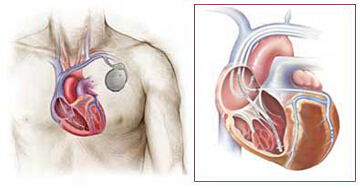
明显的三尖瓣反流(TR)在心脏衰竭(HF)患者较为常见,并且预示者较差的预后。近日,心血管领域权威杂志Eur Heart J-Card Img上发表了一篇研究文章,研究人员试图明确较差的预后是否来自于TR本身,以及TR是否是晚期左侧心肌或心脏瓣膜疾病的标志。
研究人员分析了639例急性心衰患者。对多个临床和超声心动图参数进行调整后,研究人员评估了TR严重程度与HF再入院或死亡终点之间的关系。TR等级较高与较高的充血评分以及其他心脏异常相关,这些异常包括左室收缩功能降低、中度或重度二尖瓣返流、肺动脉高压(PH,定义为肺动脉收缩压≥50mmHg)和右心室功能不全(P均<0.001)。
由此可见,伴有症状性HF和显著TR的患者存在多种并存的心脏异常。TR在正常或轻度升高的肺动脉压力的患者中TR并没有增加额外的风险。但是,它与PH患者的再住院和死亡率相关。
原始出处:
Diab Mutlak,et al.Tricuspid regurgitation in acute heart failure: is there any incremental risk?Eur Heart J-Card Img. 2018. https://doi.org/10.1093/ehjci/jex343
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#急性心力衰竭#
37
#ART#
47
#三尖瓣反流#
48
#HEART#
52
#反流#
34
#三尖瓣#
34
学习了.谢谢分享
66