Nature Medicine:人类首次描绘月经周期中子宫内膜单细胞转录组图谱
2020-09-16 生物世界 Bio生物世界
人类的月经周期,就是每月一次的子宫内膜(endometrium)的脱落、再生和重塑的过程。该研究使用单细胞测序技术,系统地表征了月经周期这一人类独特的生理过程。
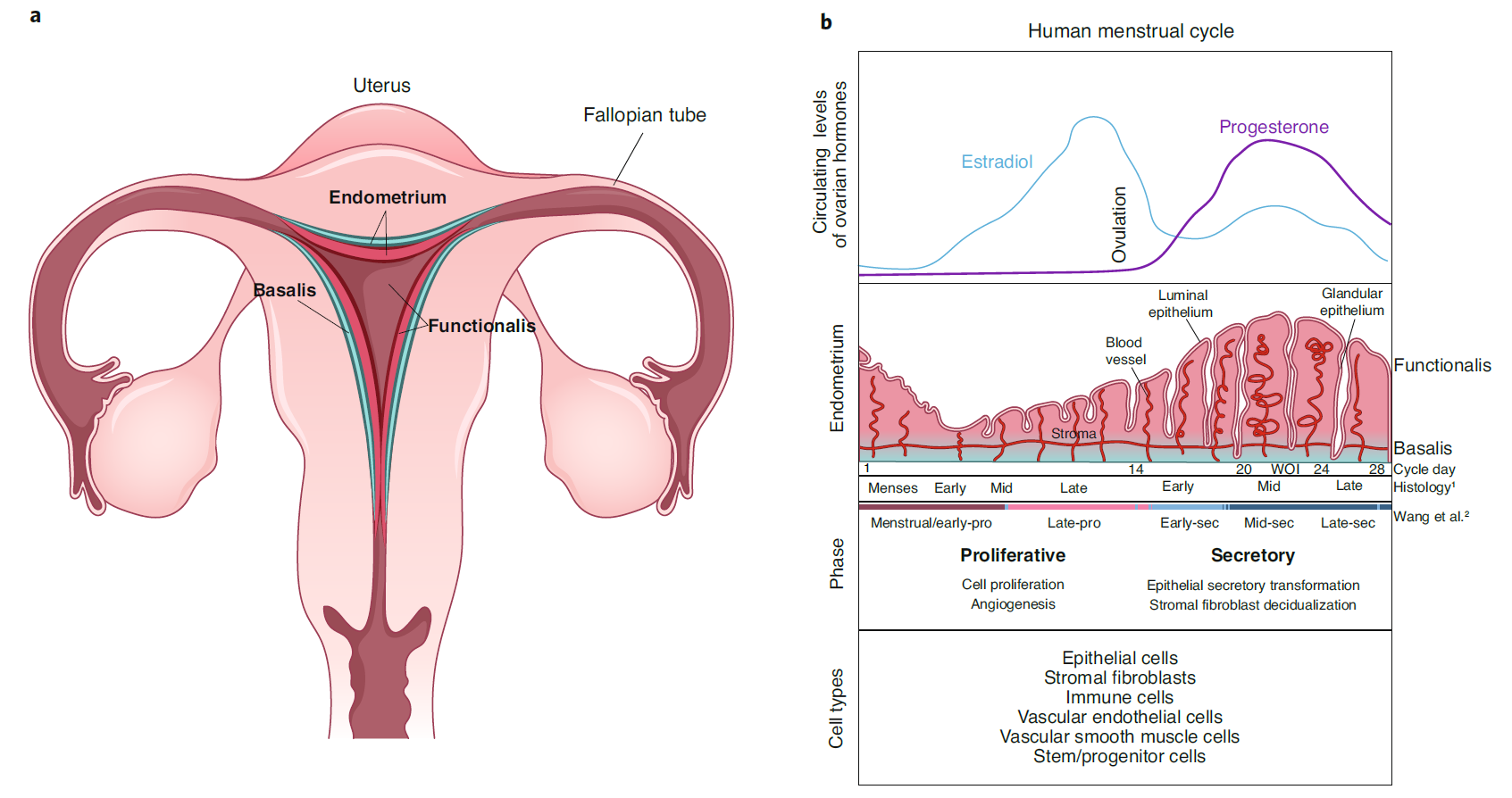
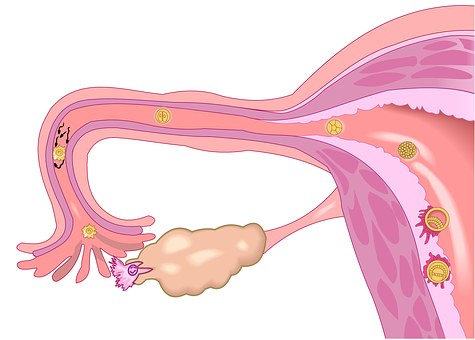
人类的月经周期,就是每月一次的子宫内膜(endometrium)的脱落、再生和重塑的过程。这一现象几乎只在人类中出现,除了人类以外,只有类人猿、旧大陆猴等极少数动物中有类似现象。
一个月经周期可以分为两个阶段:增生期(排卵前)和分泌期(排卵后),在分泌期,子宫内膜进入狭窄的接受状态窗口,此时是胚胎最佳“着床窗口”(WOI),此时子宫内膜的状态在结构和生理生化上都是理想状态。
子宫内膜不同于任何其他组织,它由多种细胞类型组成,这些细胞在一个月的周期中会经历剧烈且快速的变化,由于子宫内膜的这种周期性变化对于人类生育能力和再生生物学都有很大相关性,因此,科学家长期以来一直在寻求对整个月经周期子宫内膜转化的系统表征。然而,目前人类对月经周期中子宫内膜变化的机制理解仍然非常有限。
2020年9月14日,美国斯坦福大学的研究人员在国际顶尖医学期刊 Nature Medcine 杂志发表了题为:Single-cell transcriptomic atlas of the human endometrium during the menstrual cycle 的研究论文。
该研究使用单细胞测序技术,系统地表征了月经周期这一人类独特的生理过程。通过单细胞转录组分析,可在分子和定量水平将月经周期分为四个主要阶段,并且能够更精确地确定胚胎“着床窗口”。
子宫内膜单细胞水平的分子和基因组分析有助于理解女性生育能力、妊娠及常见疾病,将加速阐明这些疾病的发病机理,并开发出新颖的诊断方法和治疗方法,为女性健康开辟了新前景。
王宛欣 和 Felipe Vilella,为该研究的共同第一作者,Carlos Simon 和 Stephen R. Quake 为该研究的共同通讯作者。
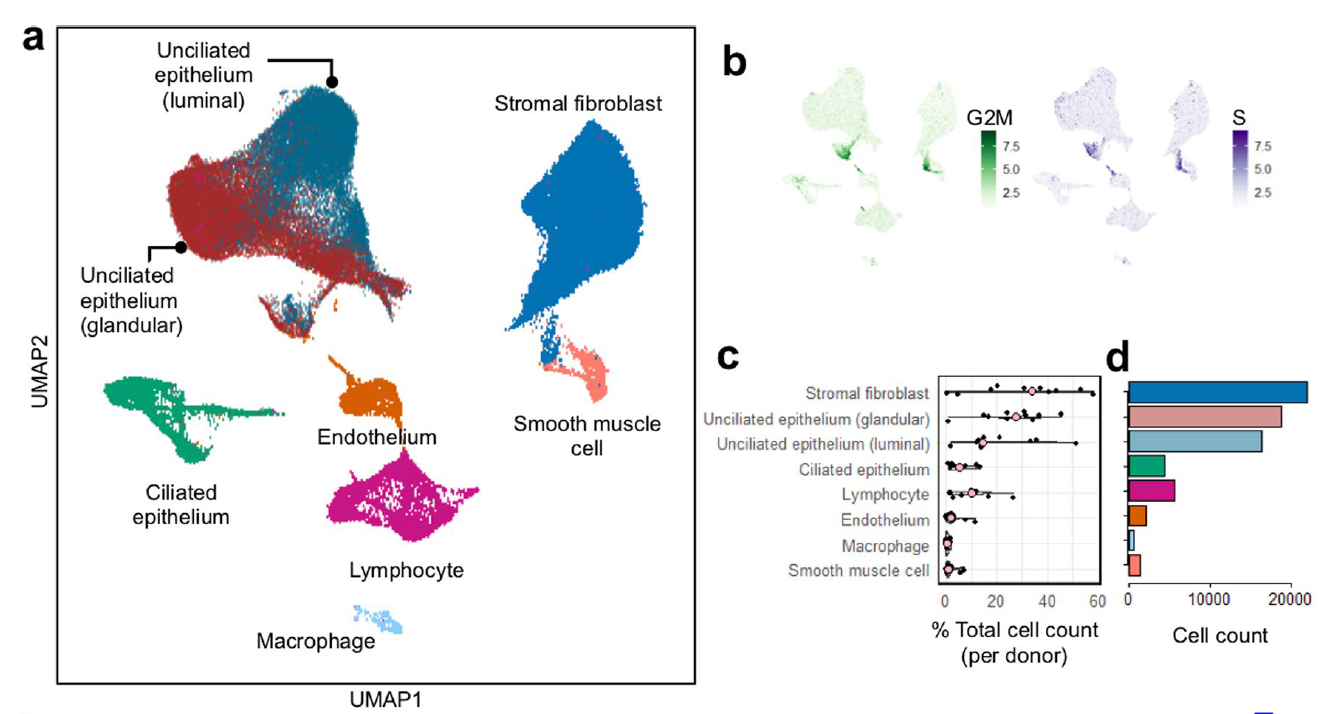
研究团队使用两个不同的单细胞测序平台分析了29位不同女性的子宫内膜活检,每个女性在月经周期进行了一次采样。整个转录组无偏见分析了子宫内膜的主要细胞类型:上皮细胞、成纤维细胞、内皮细胞、免疫细胞和干/祖细胞。
由于女性的月经周期长度各不相同(通常为24-35天),并且子宫内膜细胞的类型和数量在整个周期内也各不相同,因此将分子分析“定时”到月经周期中特定时间或阶段难以实现。
为了解决这一难题,研究团队开发了新模型,对子宫内膜组织中最丰富的两种细胞类型:纤毛上皮细胞和基质成纤维细胞的全基因组转录组数据进行了高维数据的降维分析。
研究团队发现,通过转录组分析,人类月经周期可分为四个主要阶段:月经及增生早期、增生后期、分泌早期、分泌中后期。
总体来说,月经周期中的四个阶段之间的转化基本呈连续状态,但第三阶段(分泌早期)到第四阶段(分泌中后期)的转化显然并不连续,纤毛上皮细胞转录组变化剧烈,而第四阶段的特征与“着床窗口”相吻合。
这些发现表明,“着床窗口”打开时,会发生纤毛上皮细胞转录组特征突然变化,而基质成纤维细胞就没有这种剧烈变化。

由于子宫内膜组织学不足以预测对子宫内膜胚胎植入的接受性,因此在临床上,已将子宫内膜活检的组织转录组学分析用于对接受体外受精的部分女性进行胚胎移植时判断“着床窗口”的计时。
该研究可以通过纤毛上皮细胞转录组特征变化,以单细胞分辨率来确定“着床窗口”,丰富了子宫内膜不育及相关疾病的未来临床诊断和靶向治疗。
人子宫内膜的另一种主要细胞类型——基质成纤维细胞,这些细胞对孕酮激素的反应,称为蜕膜化(decidualization),导致免疫细胞群的募集和血管生成,这对于成功怀孕至关重要。之前认为人类与其他物种不同,人类的蜕膜化与妊娠无关。
然而,这项研究表明,在非妊娠状态下,基质成纤维细胞相对于妊娠早期蜕膜中的成纤维细胞具有独特的特征,这表明妊娠可能影响成纤维细胞的蜕膜化。
此外,免疫细胞在子宫内膜功能、妊娠以及子宫内膜组织脱落和再生中起关键作用。该研究发现了在月经周期的不同阶段子宫中自然杀伤细胞的转录组变化和淋巴细胞的变化。
通过单细胞测序分析可提供有关子宫内膜细胞谱系分化以及组织再生和修复的基础机制信息。此外,空间转录组学有望提供对子宫内膜小生境的深入了解,而超越转录组学的单细胞测序分析将促进细胞过程的解构,包括解析最近在子宫内膜上皮细胞中发现的癌症驱动基因突变的作用。
在临床上,子宫内膜在女性的生育能力、妊娠以及女性常见疾病(包括子宫内膜异位,子宫腺肌病,异常子宫出血和子宫内膜癌)中起主要作用。
子宫内膜单细胞水平的分子和基因组分析将加速阐明这些疾病的发病机理,并开发出新颖的诊断方法和治疗方法,以取代目前各种激素疗法和手术疗法。
总的来说,这是第一个成功应用单细胞测序技术系统表征女性子宫内膜随月经周期变化的研究,这项研究为女性健康开辟了新的前景。
原始出处:
Wanxin Wang, Felipe Vilella, Pilar Alama, et al.Single-cell transcriptomic atlas of the human endometrium during the menstrual cycle.nature medicine.Published: 14 September 2020
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
.JPG)










🐂
63
#转录#
35
#DIC#
32
#Nat#
28
#转录组图谱#
30
#CIN#
32
#内膜#
28
#月经#
39
#转录组#
39
#Medicine#
34