诊断试验中单个ROC面积估计的样本量计算
2018-11-29 陶立元 赵一鸣 临床流行病学和循证医学
在诊断性研究中我们经常会用到AUC这个指标,即曲线下面积,它反映了一个诊断指标的总体诊断价值如何,我们也经常通过比较两个不同的指标的AUC大小及其差异是否有统计学意义,来反映这两个指标中那个指标的的诊断能力更强。在诊断性研究中我们有可能提出一个新的诊断指标,它的诊断准确性可能比既往的已经存在的诊断方法的诊断准确性要高。为了研究这个新的诊断指标的诊断价值是否比既往的诊断指标要好,我们需要设计一个试验
在诊断性研究中我们经常会用到AUC这个指标,即曲线下面积,它反映了一个诊断指标的总体诊断价值如何,我们也经常通过比较两个不同的指标的AUC大小及其差异是否有统计学意义,来反映这两个指标中那个指标的的诊断能力更强。
在诊断性研究中我们有可能提出一个新的诊断指标,它的诊断准确性可能比既往的已经存在的诊断方法的诊断准确性要高。为了研究这个新的诊断指标的诊断价值是否比既往的诊断指标要好,我们需要设计一个试验进行探索,那么这个试验的样本量应该如何计算呢?除了这个已经存在既往的诊断方法AUC外,我们还可能遇到需要检验某个新的诊断方法的AUC是否大于0.5且差异有统计学意义的情况。本次我们就使用PASS 11.0软件来进行这两种情况下的样本量估计。
在PASS 11.0中你需要打开“TestsFor One Roc Curve”这一计算过程,如下图中红圈:

打开后,对话框如下如:

例1:需要检验某连续性指标的诊断AUC是否大于0.5,根据既往信息得知该AUC为0.75,取beta=0.1,alpha=0.05,病例组与对照组样本例数相等,双侧检验。则在上述图中依次填写:Power=0.9, alpha=0.05, N-=use R, R=1, AUC0=0.5, AUC1=0.75, LowerFPR=0.00, Upper FPR=1.00, type of data=continuous, AlternativeHypothesis=two-sided test.
然后点击Run,计算结果如下图,提示每组需要研究对象25例。

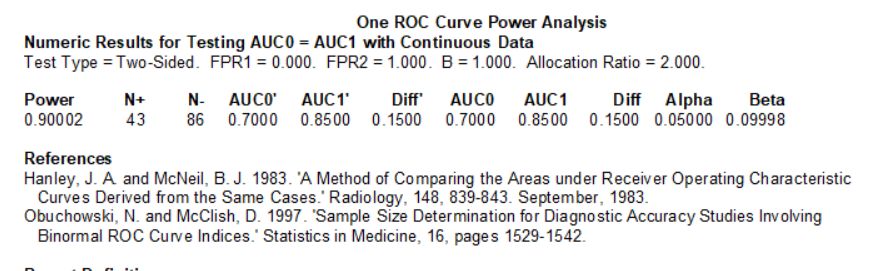
例2:需要检验某连续性指标的诊断AUC是否大于0.7(0.7为既往的已经存在的诊断方法的AUC),根据既往信息得知该AUC为0.85,取beta=0.1,alpha=0.05,病例组与对照组样本例数比例为1:2,双侧检验。则在上述图中依次填写:Power=0.9,alpha=0.05, N-=use R, R=2, AUC0=0.7, AUC1=0.85, Lower FPR=0.00, Upper FPR=1.00,type of data=continuous, Alternative Hypothesis=two-sided test.
然后点击Run,计算结果如下图,提示病例组需要研究对象43例,对照组需要研究对象86例。
另外,需要注意的是上述均是对连续性指标的AUC估算,如果不是对连续性指标,而是离散型指标(如取值仅为1,2,3,4,5,6)的情况。则需要对上述参数中的Lower FPR和Upper FPR进行调整,FPR是假阳性率即1-特异度。在连续性指标中Lower FPR必须填写0.00,UpperFPR必须填写1.00;而在离散型指标中这两个数值则是可以变化的,如果不是0和1,则表示计算的AUC不是全部曲线下面积,而是有所缩减的。
同时在对离散型数据进行计算时,我们还需要填写B值,B值等于阴性组取值的标准差除以阳性组取值的标准差,我们一般假设阴性组和阳性组的取值均是正态分布的(即双正态分布),但是实际工作中离散型数据更不容易符合这一特征。Obuchowski等人的研究指出B值一般小于1,在0.3附近。但是她也建议如果我们无法很好的估计B值时可以直接取1,这样计算出的样本量最大,也更为保守。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#诊断试验#
35
#样本#
28
#ROC#
29
#样本量#
39