JAHA:发热与ST段抬高型心梗患者预后呈显著相关
2017-07-23 MedSci MedSci原创
双相炎症反应在ST段抬高型心肌梗死(STEMI)后的心肌愈合和全身动脉粥样硬化的进展中起重要作用。近日,在国际心血管权威杂志JAHA上发表了一篇旨在评估STEMI后第一和第二炎症时相的发热对心脏远期预后影响的临床研究。本研究共纳入了550名ST段抬高型心肌梗死的患者。对纳入的研究对象测量腋下的体温,并分别测量记录第一时相(入院后3天内,max‐BT1-3d)和第二时相(入院后4-10天,max‐B
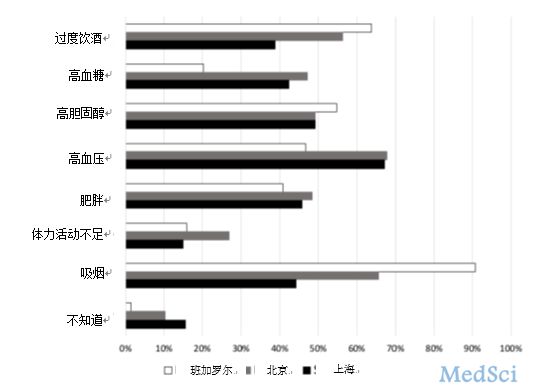
双相炎症反应在ST段抬高型心肌梗死(STEMI)后的心肌愈合和全身动脉粥样硬化的进展中起重要作用。近日,在国际心血管权威杂志JAHA上发表了一篇旨在评估STEMI后第一和第二炎症时相的发热对心脏远期预后影响的临床研究。本研究共纳入了550名ST段抬高型心肌梗死的患者。对纳入的研究对象测量腋下的体温,并分别测量记录第一时相(入院后3天内,max‐BT1-3d)和第二时相(入院后4-10天,max‐BT4-10d)的患者最高体温。之后,对患者进行长达平均5.3年的随访,随访内容主要是心脏不良事件,包括心源性死亡、急性冠脉综合征和心衰源性的再住院率。在随访期间,有80名患者经历了心脏不良事件。研究结果显示,高的max‐BT4-10d与患者远期的心脏不良事件发生呈强相关,max‐BT4-10d每升高1℃的HR为2.834,95% Cl为2.017-3.828,p<0.0001,而max‐BT1-3d与心脏不良事件的发生无显着相关性(1.136 [0.731-1.742], P=0.57)。即使将冠状动脉危险因素进行调整后,包括肾小球滤过率、梗死面积、心包积液和出院药物,第二时相的发热(m
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#心梗患者#
32
#ST段抬高型心梗#
42
#患者预后#
37
#AHA#
23
#ST段抬高#
36
#ST段#
28