JCI:siRNA筛选发现促乳腺癌转移关键因子
2015-03-23 佚名 生物谷
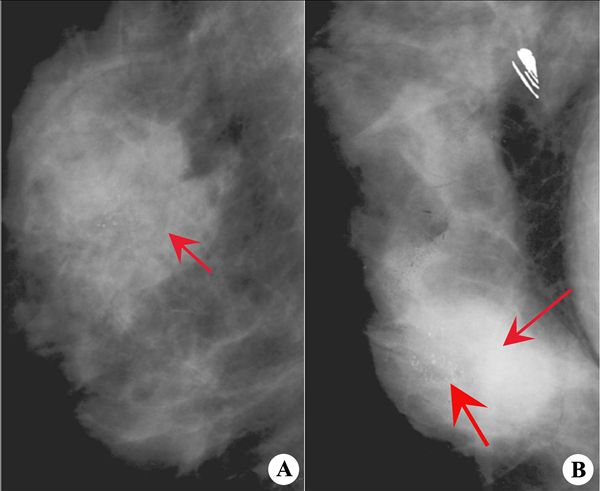
近日,著名国际期刊JCI在线发表了荷兰莱顿大学研究人员的一项最新研究成果,他们利用小干扰RNA对H1299细胞内与细胞迁移有关的基因进行了筛选,发现了一些与肿瘤细胞迁移速度和持续性有关的基因,并发现了与乳腺癌病人肿瘤转移密切相关的SRPK1基因或可成为乳腺癌药物治疗的潜在靶点,因此具有重要意义。 肿瘤细胞迁移是癌细胞扩散的一个重要过程,而这一过程主要通过信号介导的细胞骨架和细
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#JCI#
28
#关键因子#
38
#siRNA#
47
#筛选#
39
#癌转移#
44